Chronic Pancreatitis : A General Overview

- Chronic pancreatitis
- 14 Aug 2023
Overview
What is Chronic pancreatitis ?
Chronic pancreatitis is a health condition where pancreatic inflammation persists and does not go away with time. And it also interferes with the organ’s ability to function properly.
The pancreas is a long, flat glandular organ found behind the stomach. It produces hormones and enzymes that are responsible for proper digestion and regulation of blood glucose. Any persistent inflammation may lead to irreversible damage to this organ in chronic pancreatitis. Affected individuals may have gone years without showing any symptoms. When they develop symptoms, they may experience instances of constant abdominal pain. Due to its interference with the organ’s normal functioning, diabetes or poor digestion may develop. 1What is Chronic pancreatitis? | Researched based study from Nih.gov Treatment can improve mild pancreatitis, but life-threatening complications can result from severe cases.

Causes
Causes
It is a multifactorial disease that can be caused by any of the following:
- Genetic reasons – Hereditary pancreatitis, cystic fibrosis, etc.
- Alcohol abuse – About 70% of cases had an alcohol consumption element.
- Repeated acute pancreatitis – causes chronic pancreatitis by permanently damaging the organ.
- Autoimmune diseases – Celiac diseases 2Causes | Researched based study from Nih.gov such as autoimmune pancreatitis or systemic lupus erythematosus (SLE).
- Ductal obstruction – due to small ducts, cancer, trauma, gallstones, or pancreatic stones.
- Chemotherapy – Pancreatitis can be brought on by chemotherapy. 3Causes | Researched based study from Springer.com
- Hypertriglyceridemia – a heavy amount of blood triglyceride fats.
- Idiopathic – Sometimes a cause of pancreatitis is never identified.
- Hypercalcemia – blood calcium levels are elevated.
Risk
Risk factors
A person’s chance of getting chronic pancreatitis may be increased by the following elements:
- Hereditary – The likelihood is increased when a family member has this disorder, especially when other risk factors are present.
- Age – Occurs more frequently in adults aged 30 to 40.
- Gender – More males than women experience this.
- Heavy alcohol consumption – the danger is higher for heavy drinkers. 4Risk factors| Researched based study from Nih.gov
- Cigarette smoking – Compared to nonsmokers, smokers have a three times higher risk of developing chronic pancreatitis. When mixed with alcohol, the risk is doubled.
- Obesity – Obese individuals are more susceptible to the disease.
- Diabetes – Diabetic patients are more at risk.
Symptoms
Symptoms
In the initial stages, the patient may not experience any symptoms and with disease progression, changes in the pancreas can make the patient feel unwell. Symptoms may include:
- Sudden, severe, or minor episodes of abdominal pain.
- Some may have persistent pain.
- Upper abdominal discomfort.
- Pain that worsens after consuming alcohol or eating certain foods.
- Yellowish discoloration of the skin and eyes.
- Having a bad feeling.
- Prolonged diarrhea.
- Weight reduction.
- Vomiting and nauseous.
- glucose intolerance.
- greasy stools.
- Breathlessness.
- Extreme thirst.
- Exhaustion.
- Backache.
Prevention
Prevention
The following steps may help avoid pancreatitis to some extent:
- Cut back or stop drinking alcohol 5Prevention | Researched based study from Nih.gov
- Work out regularly.
- Quit smoking.
- Keep your weight in check.
- Eat a diet rich in fruits and vegetables that is well-balanced.
- Avoid eating fatty, cholesterol-rich foods.
- Increase consumption of dietary fiber.
- Avoid taking drugs that are known to induce acute pancreatitis.
Complications
Complications
The following are possible pancreatitis complications:
- Kidney failure.
- Pseudocysts – are risky because they can obstruct vital blood arteries and channels. In some circumstances, they may become infected as well.
- Splenic venous thrombosis – Blood clots form in the splenic vein.
- Pancreatic ascites (rare) – Juices from the pancreas gather in the abdomen. 6Complications | Researched based study from Nih.gov
- Pleural effusion (rare) – a fluid accumulation around the lungs.
- Pseudoaneurysms (rarely of the vessels close to the pancreas) – blood seeps from the vessel and collects in the tissue around it.
- Recurrent acute pancreatitis, particularly in drinkers who do not abstain from alcohol.
- Nutrient malabsorption – It is one of the most frequent consequences. The body is not properly absorbing nutrients as a result of insufficient production of digestive enzymes by the affected pancreas.
- Diabetes – can be caused by damage to the insulin-producing cells of the pancreas. Diabetes may develop in about 45% of those with chronic pancreatitis.
- Pancreatic cancer – long-lasting pancreatic inflammation, increases the chance of developing the disease.
- Pancreatic calcification – Calcium salt deposits cause the tissue of the pancreas to stiffen.
- Chronic pain – makes it challenging to live a happy life.
Diagnosis
Diagnosis
To diagnose pancreatitis, a physical examination, questions regarding symptoms, drinking habits, medical and family histories, and a few tests are required:
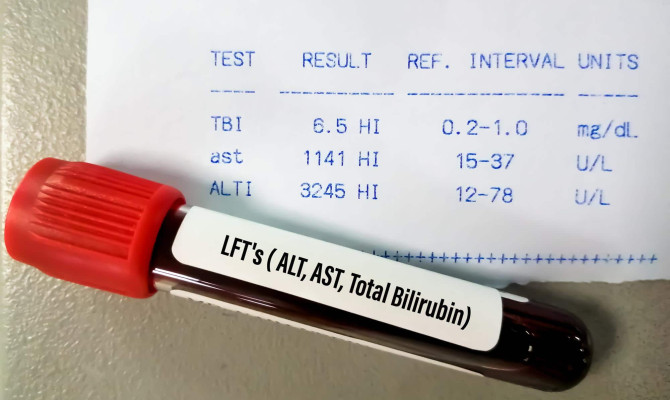
- Blood and urine tests – to look for raised white blood cell counts, kidney function, liver enzyme levels, and increased levels of pancreatic enzymes including amylase and lipase.
- Stool test – used in cases of chronic pancreatitis to assess fat levels that may indicate reduced food absorption by the digestive system.
- Abdominal ultrasound – for locating gallstones and other obstructions.
- Computed tomography (CT) – used to identify gallstones and estimate the severity of pancreatic inflammation.
- Magnetic resonance imaging (MRI) – to check for any ductal, pancreatic, or gallbladder defects.
- Endoscopy – to check the anatomy of the pancreas in great detail, along with any cysts, blockages, narrowing, or ruptures.
- Endoscopic ultrasonography – to check for bile or pancreatic duct obstructions and swelling.
Treatment

Treatment of Chronic pancreatitis
The following are some examples of treatment options for chronic pancreatitis, which focus on relieving pain and enhancing digestive function:
Medications:
- Painkillers – Paracetamol or anti-inflammatories like ibuprofen are typically the first drugs used.
- Strong painkillers – One could require an opiate-based painkiller, such as codeine or tramadol if the first drug of choice does not control pain.
- Severe pain – It might be advised to take medications like gabapentin, amitriptyline, or pregabalin. May also be referred to a pain center.
- Nerve blocks – a nerve block injection may be used temporarily to ease severe pain for weeks or months.
- Enzyme supplements – to improve the efficiency of the digestive system.
- Insulin – provided in pancreatic diabetes.
- Steroid medicine – is advised for those with chronic pancreatitis brought on by immune system issues.
- In cases of malnutrition, vitamins or mineral supplements.
Surgical management:
It is opted when the pain is not responding to medication and may include:
- Cholecystectomy – could be beneficial in recurring cases and is done to remove the gallbladder.
- Pancreatic sphincteroplasty – performed to rebuild the muscle of the pancreatic sphincter.
- Endoscopic surgery and lithotripsy – may be beneficial to individuals who have stones at the entrance of their pancreatic duct. Although the discomfort may be somewhat reduced as a result, the effect might not last forever.
- Pancreas resection – It is the surgical removal of specific, painfully inflamed pancreatic parts.
- Total pancreatectomy – when there has been significant damage, the entire pancreas is removed. This can be a very effective way to relieve pain. Long-term supplementary insulin therapy or a procedure called as autologous pancreatic islet cell transplantation (APICT) may be utilized to solve this issue.
- Surgery may also be done to remove dead tissue or to drain fluids.
Other treatment:
- Alcohol de-addiction – In many circumstances, enrolling in a program to treat alcohol addiction might help the situation improve.
- To treat acute pancreatitis or a flare-up, the patient may need to stay in the hospital. Treatment options include fasting, intravenous fluids, painkillers, and tube feeding.
Remedies
Home remedies:
- Stay away from alcohol – Enrolling in an alcohol deaddiction program may help.
- Quit smoking – Some medication and therapy may help.
- Eat a low-fat diet – Choose a diet that prioritizes lean protein, nutritious grains, fresh produce, and little to no fat.
- Increase daily fluid intake – Drink additional water throughout the day because pancreatitis can lead to dehydration.
- Exercise regularly to maintain a healthy weight.
- Combine other methods to cope with pain like meditation, mindfulness, yoga, breathing exercises, acupuncture, etc.
Diet
Dietary tips for recovery
When a person has chronic pancreatitis, it is preferable to speak with a dietitian before making dietary changes. The following are a few tips:
- Consume 6 to 8 small meals throughout the day to aid with pancreatitis recovery as it is a simpler load for the digestive system.
- Include vegetables, fruits, whole grains, lentils, and beans.
- Include fish like cod, haddock, etc.
- Include lean meat, such as turkey or chicken.
- For the daily nutrient requirement, take a multivitamin dietary supplement.
- Because MCTs (medium chain triglycerides) do not require pancreatic enzymes to be absorbed, use them as the main source of fat. MCTs can be found in coconut oil.
- Limit the amount of fiber consumption at once to prevent slowing digestion and nutrient absorption. Moreover, fiber can reduce the efficiency of the only few enzymes that the affected person may have.
- Avoid fried food.
- Avoid alcohol as an ingredient in the food.
Takeaway
Key Takeaways
It is impossible to reverse pancreatic damage, but most of the symptoms could be managed if they are treated properly. Once diagnosed with chronic pancreatitis, it is advisable to stay away from alcohol to avoid serious complications including death. Also, as smoking increases the risk of developing pancreatic cancer, it should be avoided. There is an increased risk of death for people who need surgery for a pseudoaneurysm. 7Key Takeaways | Researched based study from Nih.gov The prognosis is based on how bad the condition is, what the underlying cause is, your age at diagnosis, the amount of alcohol you continue to consume, and whether you continue to smoke can all have an impact on your chances of recovery. An improved treatment outcome can result from quick diagnosis and treatment.
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
National Institutes of Health
Chronic Pancreatitis | Overview
-
National Institutes of Health
Patients with Celiac Disease Have an Increased Risk for Pancreatitis
-
Springer Nature
Cancer therapy related complications in the liver, pancreas, and biliary system: an imaging perspective
-
National Institutes of Health
Myths and Realities about alcohol and smoking in chronic pancreatitis
-
National Institutes of Health
Global epidemiology and holistic prevention of pancreatitis
-
National Institutes of Health
Pancreatic Ascites | Complications
-
National Institutes of Health
Surgical treatment of pain in chronic pancreatitis