What is Osteoporosis: Diagnosis, Treatment and Prevention

- Osteoporosis
- 17 Aug 2023
Overview
What is Osteoporosis?
Osteoporosis is a disease of the bones. It occurs as a result of too much bone loss from the body or too less production of bone. Thus, making the bones weaker.
Bones that have osteoporosis are fragile and are readily broken. Osteoporosis is referred to as a “silent disease”.
Nearly 54 million Americans 1Overview| Researched based study from Bonehealthandosteoporosis.org experience osteoporosis and less bone mass. This puts them at increased risk for osteoporosis.

How does osteoporosis occur?
- A bone is naturally made of calcium salts, minerals and collagen fibers. The hard outer covering of the bone is called cortical bone. The soft mesh of spongy bone is called trabecular bone.
- Bones are active and living tissues of the body that renew themselves constantly. Old tissue of the bone is broken down by osteoblastic cells and replaced by newer bone material produced by osteoblastic cells.
- The literal identification of osteoporosis is “porous bone”.
- When you view the bone under a microscope, healthy bones resemble a honeycomb. In case of osteoporosis, the spaces and holes in the honeycomb appear larger than the ones in healthy bones. The upper shell or layer of bone also gets crushed. All these events contribute in making the bone weaker.
Causes
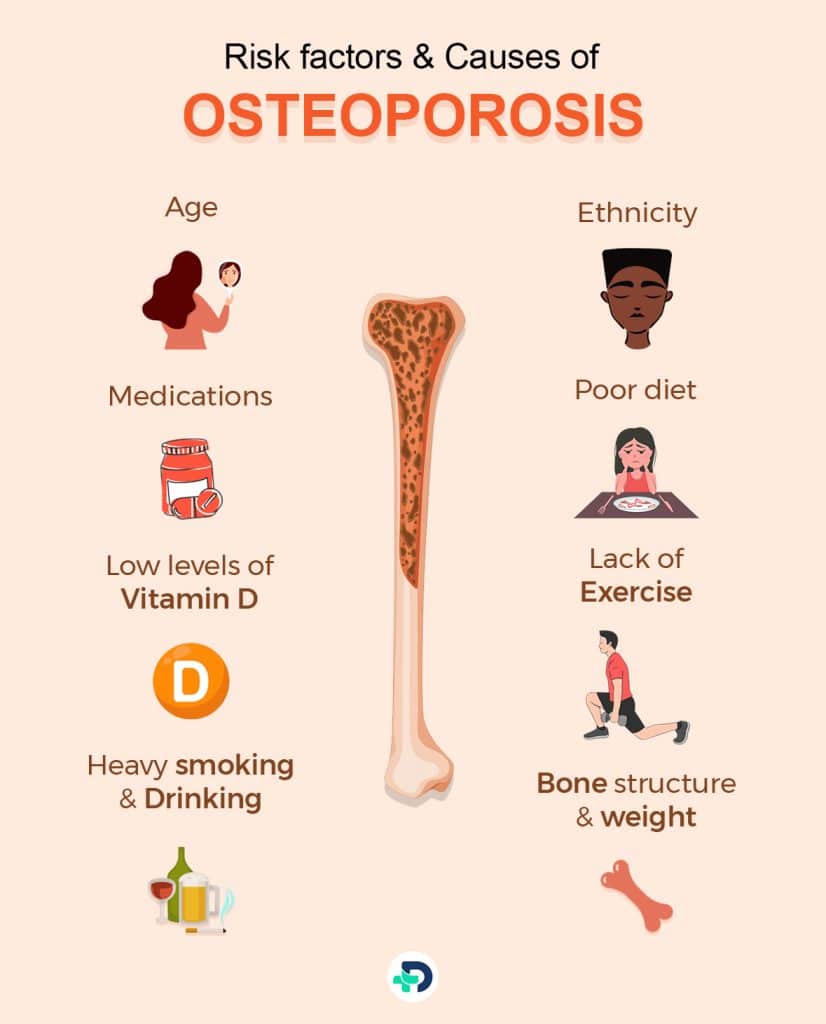
Risk factors and Causes of Osteoporosis
There are few risk factors that increase the chance of developing osteoporosis:
- Increase in age
- Ethnicity
- Weight & Structure of bone
- Existing health condition
- Medicines
- Family history
- Poor diet
- Vitamin D deficiency
- Drinking & Smoking
- Pregnancy & Lactation
- Gastrointestinal Surgery
Age
- Estrogen and testosterone are the sex hormones 2Causes| Researched based study from Betterhealth.vic.gov.au that play a crucial role in preserving bone density and bone strength in both genders. The fall in estrogen levels at age of 50 or that occurs during menopause results in a significant reduction in bone density. In the initial five years following menopause, a female experiences a reduction of up to 10% in her overall body bone mass.
Ethnicity
- Caucasian and Asian women are more susceptible to suffer from osteoporosis.
Bone structure and weight
- People with lean bodies and lower body weight are at an increased risk of osteoporosis due to lower bone mass in comparison to those with larger body weight and frames.
Medical conditions
Any condition that alters your hormone level has the ability to cause osteoporosis.
It can be:
- Hyperthyroidism
- Para-thyroidism
- Overactive adrenal glands
- History of organ transplant
- Hormonal treatment for breast/prostate cancer
- Inflammatory bowel disease
- Multiple myeloma
- History of bariatric surgery
- Gastrointestinal bypass procedures
- Stroke
- Spinal cord injuries
- Low levels of testosterone and estrogen in men
- AIDS/HIV
- Parkinson’s disease
- Multiple sclerosis (MS)
- Chronic kidney disease
- Liver disease.
- Polio
- Chronic obstructive pulmonary disease (COPD)
Medications
Some medications 3Causes| Researched based study from Nhs.uk like steroids, drugs used in the treatment of breast cancer and the drugs used for treating seizures have the tendency to cause osteoporosis.
The following drugs may cause bone loss:
- Antacids
- Cyclosporine A and FK506 (Tacrolimus)
- Heparin
- Anti Seizure medicines (only some) such as Dilantin® or Phenobarbital
- Aromatase inhibitors such as Arimidex®, Aromasin® and Femara®
- Cancer chemotherapeutic drugs
- Lithium
- Gonadotropin releasing hormone (GnRH) such as Lupron® and Zoladex®
- Selective serotonin reuptake inhibitors (SSRIs) such as Lexapro®, Prozac® and Zoloft®
- Proton pump inhibitors (PPIs) such as Prevacid® and Nexium®
- Medroxyprogesterone acetate in case of contraception (Depo-Provera®)
- Methotrexate
Low levels of Vitamin D
- Vitamin D helps in calcium absorption and maintenance of adequate calcium levels that are required for mineralization of bones. Vitamin D promotes bone growth and remodeling. The deficiency of Vitamin D accelerates bone loss, bone turnover and bone fractures.4Causes| Researched based study from Nlm.nih.gov
Lack of exercise
- Regular Exercise aids in the development of bones. Lack of exercise determines more loss of calcium from the bones resulting in osteoporosis.
Poor diet
- You are more likely to develop osteoporosis if your diet is deficient in vitamin D or calcium, or if your body mass index is low.
Family history
- Osteoporosis is a hereditary condition that is caused because of inherited genetic factors. These factors will have an impact on the development of the bones. If someone from your family has suffered a osteoporotic fracture then your risk of a fracture is greater than normal.
Heavy smoking & Drinking
- Tobacco in cigarettes is highly toxic to bones. In females it lowers the estrogen level and can lead to early menopause. In males, smoking decreases the testosterone activity and can weaken the bones.
- Alcoholism suppresses the ability of the body to make bones. It also elevates the risk of fracture due to fall.
Gastrointestinal surgery
- Bariatric surgery is known to reduce the stomach size thus limiting the intestinal surface area. This causes a fall in calcium absorption and other nutrients. Osteoporosis occurs when there is less bone mass density.
Pregnancy and Lactation Associated Osteoporosis (PLO)
- Temporary bone density loss is a physiological issue in pregnancy and lactation. Fractures are very uncommon during this period. PLO can be brought on by hip fractures, spine fractures accompanied with back pain etc.
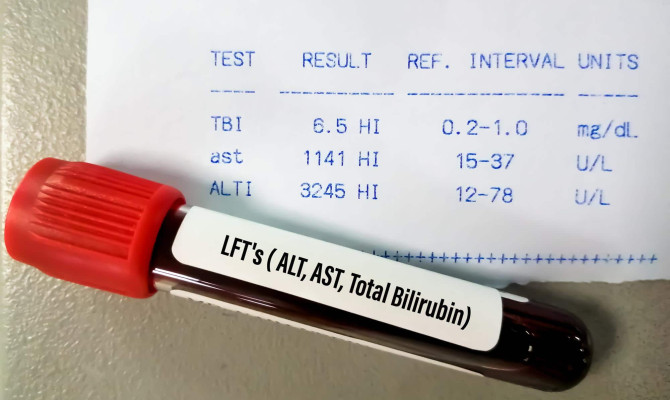
Diagnosis
Diagnosis of Osteoporosis
The most widely accepted test for the measurement of bone mineral density is dual-energy x-ray absorptiometry (DXA).
Bone density tests 5Diagnosis| Researched based study from Mayoclinic.org are performed on the bones that are susceptible to break including:
- Lower spine bones (lumbar vertebrae)
- Neck of your thigh bone (femur)
- Forearm bones
- Hip joint
DXA scan
- It is a painless and quick scan test. It is also non invasive and utilizes minimal levels of X-rays as it scans the body. It takes around 10-30 minutes only.
- The test measures bone density at the hip and spine which is the most reliable method for the diagnosis of osteoporosis.
- Peripheral DXA scan measures bone mineral density (BMD) at the wrist and heel.
- The doctor will thoughtfully evaluate your BMD results with the mean bone density of healthy people.
You must get this scan done if
- You Are on steroid medications for three months or more.
- You have had a low impact fracture.
- You experienced early menopause.
- There is a history of hip fracture in your family.
- Medical conditions that affect the bones like rheumatoid arthritis, hyperthyroidism, inflammatory ball, disease, or diabetes.
- Your BMI (body mass index) is less than 19.
Quantitative ultrasound (QUS)
- Quantitative ultrasound of the heel is done for bone evaluation only. It doesn’t measure bone mineral density (BMD). If the QUS shows bone loss then DXA scan is done for further analysis.
T- score
- Your T-score is your bone density compared with the normal as in a healthy young adult male/female.
- Your T-score gives the unit number that shows whether the density of bones is above or below the average.
CT scan
- It is done to know the underlying cause of osteoporosis. It detects bone disorders, location of bone infections, internal injuries etc.
Treatment
Treatment of Osteoporosis
Treatment modalities are based upon the risk of bone breaking using the information from the bone density test. Few treatment lines are:
Bisphosphonates
- The most commonly prescribed medications for Osteoporosis are bisphosphonates, for both males and females who are at increased risk of fracture.
- Examples include Alendronate, Risedronate, Ibandronate and Zoledronic acid
Denosumab
- Compared to bisphosphonates, denosumab (Prolia, Xgeva) gives satisfying bone mineral density results. It also reduces the likelihood of all kinds of fractures.
- It is given subcutaneously every six months.6Treatment| Researched based study from Mayoclinic.org
Hormone-related therapy
- Estrogen therapy as soon as after menopause will help in the maintenance of bone mineral density.
- Estrogen derived drug, Raloxifene (Evista) has good results of BMD in postmenopausal women. This drug is also used for decreasing the prevalence of a few types of breast cancer. The bone density must begin to improve after 6 to 12 months of starting this treatment.
- Decline in the levels of testosterone in men with gradual aging is the prevalent factor for osteoporosis. It can be improved by giving testosterone replacement therapy.
Osteoclastic medications
- Severe osteoporosis can be treated by using Teriparatide, Abaloparatide and Romosozumab
Pain relief OTC drugs
It’s expected that you will require pain relief medications, for example:
- Painkillers (analgesics): Paracetamol, occasionally morphine and codeine.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Ibuprofen or naproxen.
Calcitonin
- It is usually used for preventing loss of bone density. Calcitonin is for short-term treatment of Osteoporosis. Calcitonin is used in case of immobilization after an osteoporotic fracture.
- It can be given subcutaneously or intramuscularly. Nausea, headache, distaste, musculoskeletal, pain and diarrhea are a few of the possible side-effects.
RANK ligand (RANKL) inhibitor
It helps in slowing down loss of bone density. It is approved for treatment of osteoporosis in:
- Osteoporosis in postmenopausal women
- Men who have low BMD and are getting treatments for prostate cancer.
- Women who have low BMD and are getting treatments for breast cancer.
- Patients who show no response to other types of osteoporosis treatment.
Sclerostin inhibitor
- It is a medication that cures severe osteoporosis. It works by inhibiting the action of a protein. Sclerostin inhibitor encourages the body to elevate new bone formation along with slowing down bone loss.
When should you use medications for treatment of Osteoporosis?
- Females having bone density tests that show T-scores of -2.5 or less, such as -3.3 or -3.8, must start therapy to decrease their risk of fracture. Few females require proper management if they have osteopenia. Osteopenia means bone weakness which is not so severe as osteoporosis.
Prevention
Prevention of Osteoporosis
Strong defense mechanisms can be made to prevent Osteoporosis, like:
Diet modifications
- It is important to take recommended daily intake of calcium, vitamin D, and proteins.
- Calcium can be obtained from various sources such as low-fat dairy products, fish, leafy green vegetables, and enriched juices, milk etc.
Lifestyle
Along with a healthy diet and supplements, a good lifestyle is necessary for maintaining bone health.
You should:
- Refrain from secondhand smoke.
- Quit smoking.
- Don’t drink alcohol excessively.
- Get enough rest.
- Don’t overburden yourself with physical stress.
Regular exercise
Physical activity is an important step of an osteoporosis management plan. Exercise does not increase bone mass in older adults but regular exercise can benefit older adults such as:
- Improve muscular mass and strength.
- Improve coordination and equilibrium. Thus reducing the risk of falls.
- Enhance daily functioning of the body
Special exercises
Activities that encourage muscle strength, balance and muscle coordination like tai chi, Pilates and yoga are important, as they can aid in prevention of sudden falls by improving your balance, bone strength and maintaining posture.
- Tai chi is a Chinese martial art. Tai chi belongs to the category of “soft” martial arts. In the Western world, it is gaining more popularity as a method for managing stress and promoting exercise. Tai chi 7Prevention| Researched based study from Betterhealth.vic.gov.au comprises slow and measured movements or postures that are typically performed outdoors to absorb the outer energy of nature.
- A blend of weight-bearing and strength-training episodes in a week is apt. Aim for around 30 to 40 minutes of exercise for four to six times a week. Exercise for bone growth must be regular for better results.
Precautions
Precautions
If you have osteoporosis, the following advice along with your doctor-recommended therapies, may help you manage your condition, live with it, and reduce your risk of fractures and falls.
Below are some recommendations for reducing the risk of osteoporosis and osteoporotic fractures in outdoor settings and while traveling:
- Utilize a cane or walker to enhance stability.
- Select supportive shoes with thin, non-slip soles. Avoid wearing slippers.
- When sidewalks are slippery, it is advisable to walk on grass. During winter, you can apply salt or kitty litter on icy surfaces
Several indoor fall prevention strategies include:
- Maintain clean and uncluttered rooms, particularly floors. Do not place any electrical cords or sharps in areas designated for walking.
- Utilize carpet runners to prevent slips on smooth surfaces.
- If you have pets, you must live with more caution to prevent tripping over them.
- Do not wear any stockings, socks or slippers.
- You must only buy the carpet that has area rugs that possess non-slip material.
- Make sure you have adequate lighting in the home.
- Should have Dual sided headrails on the stairs.
- Insert grab bars in the bathroom for easy movement.
Complications
Complications of Osteoporosis
Spinal fractures due to osteoporosis can lead to complications such as:
- Back pain that starts gradually or suddenly at the level of fracture.
- Upper back hunch due to vertebral fracture.
- Loss of height because of vertebral body fracture.
- Loss of instability and mobility in the daily chores of life due to weak bones.
- Lung and heart complications because of multiple factors that cause compression of the abdomen.
- Lifetime disability.
- Neurological injury.
Outlook
The Outlook
Osteoporosis is a threatening life condition. If neglected it might lead to disability and impairment. Therefore, it is important to maintain a balanced and healthy diet, reach daily calcium levels and exercise well.
If osteoporosis has already begun then it is important to take precautionary measures and proper treatment.
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
Bone Health and Osteoporosis Foundation
What is Osteoporosis and What Causes It? | Overview
-
Better Health Channel
Osteoporosis | Causes
-
National Health Service
Osteoporosis | Causes
-
National Library of Medicine
Vitamin D Deficiency, Osteoporosis and Effect on Autoimmune Diseases and Hematopoiesis: A Review | Causes
-
Mayo Clinic
Bone density test | Diagnosis
-
Mayo Clinic
Osteoporosis treatment: Medications can help | Treatment
-
Better Health Channel
Tai chi - health benefits | Prevention