Overactive bladder: What do I need to know?

- Overactive Bladder
- 17 Aug 2023
Overview
What does an Overactive bladder mean?
Frequent and sudden urogenital urges characterize the medical condition known as overactive bladder. People with OAB may have a rash, urgent need to urinate, frequently accompanied by urinary incontinence (unwanted urine leakage), or nocturia (repeated nighttime urinating).
Millions of people worldwide are impacted by this physical illness, which ruins their routines, restricts their social interactions, and causes emotional pain.
We shall learn about its causes, symptoms, and treatments in this article.

Symptoms
Symptoms of Overactive bladder
- Urgency to urinate
- Frequent urination
- Nocturnal peeing
- Urinary incontinence
- Urge incontinence
- Urinary retention
- Emotional impact
Although individual symptoms can differ, they typically involve urinary urgency, frequency, and occasional urinary incontinence. Here are some typical signs:
Urgency
- Urinary urges that come on quickly and firmly are the main symptom. This need may be challenging to control or postpone, leaving you with a strong urge to use the bathroom immediately.
Frequency
- OAB patients could require more frequent urination than usual. In 24 hours, this may include urinating more than eight times.
Nocturia
- It alludes to the have to get up repeatedly throughout the night to use the restroom. It may cause sleep disturbances and fatigue during the day.
Urinary incontinence
- Urinary incontinence, or the involuntary flow of urinating, is another side effect of OAB. This might take place naturally or in emergencies.
Urge to urinate
- It is a particular kind connected to OAB. It happens when the urge to urinate is so intense that urine leaks out before you can get to the toilet.
Urinary incontinence
- It may occasionally be accompanied by a struggle to empty the bladder. As a result, one may feel as though they are voiding only partially or find it difficult to start urinating.
Impact on the emotions
- It may have emotional consequences, such as fear and shame, as well as a negative effect on social interactions and general quality of life3Symptoms| Researched based study from Nlm.nih.gov ,4Symptoms| Researched based study from Nlm.nih.gov
Causes
What are the causes?
Sometimes it’s hard to pinpoint the exact causes. However, several factors and underlying issues may affect the development. The following list of common grounds and contributing aspects:
- Issues with nerves or muscles
- Hormonal changes
- UTI infections
- Bladder abnormality
- Medicines
- Lifestyle factors
- Neurological disorders
Nerve or muscle issues
- OAB may result from bladder muscle or nerve dysfunction. When the detrusor muscle, which contracts to empty the bladder, is overworked, it may frequently acquire even when empty.
- In a similar manner, anomalies in the nerves that control a full bladder. Parallel to this, problems in the nerves that regulate bladder function might impair the brain and bladder’s ability to work together typically.
Hormone changes
- Bladder control can be affected by hormonal irregularities, such as a drop in estrogen levels (expected during menopause), which may worsen the symptoms.
- Decreased estrogen can cause bladder dysfunction since it keeps the pelvic muscles and urinary tract healthy.
Infections of the urinary tract
- Bladder infections, for example, can irritate the bladder lining and result in transient discomfort. Urination may become more frequent and more urgent as a result of UTIs.
Medications
- Certain drugs may interfere with bladder function and exacerbate the symptoms.
- Medications affecting bladder control include sedatives, muscle relaxants, antihistamines, diuretics, and antidepressants.
Neurological disorders
- OAB can be caused by underlying neurological problems that interfere with the bladder’s natural function.
- Conditions like Parkinson’s disease, multiple sclerosis, stroke, spinal cord injury, and diabetic neuropathy can affect the nerves that control bladder function.
Bladder abnormalities
- Bladder stones, tumors, or bladder diverticula (pouches in the bladder wall) are structural abnormalities of the bladder or urinary system.
Lifestyle factors
- Excessive alcohol or caffeine use, eating spicy or acidic meals, drinking insufficient fluids, and being overweight. These elements may irritate or or put a pressure on the bladder3Causes| Researched based study from Nlm.nih.gov ,4Causes| Researched based study from Nlm.nih.gov
Diagnosis
Diagnosis of Overactive bladder
Medical history examination
- To understand the frequency, urgency, and significance of your symptoms, the healthcare provider will go over them in depth with you. They will enquire about any further pertinent medical issues, prescription drugs, hydration intake, and personal lifestyle choices.
Voiding diary
- Tracking your urination patterns can be done by keeping a voiding journal.
- Record your fluid intake, urine frequency, volume, urinary urgency or incontinence episodes, and whether you experience nocturia (nighttime urination).
- This diary offers helpful information to evaluate the degree and pattern of your symptoms.
Physical examination
- The condition of the reproductive and urinary systems may be evaluated physically, including a pelvic exam for female patients.
- The test helps remove any pelvic floor diseases or anatomical abnormalities that might be causing the symptoms.
Urinalysis
- A quick urine test known as a urinalysis may be performed to screen for urinary tract infections (UTIs) or other abnormalities in the urine.
- It is crucial to rule out any potential underlying reasons because it may cause symptoms similar to those of OAB.
Measuring the residue after voiding
- Measurement of post-void residual (PVR) urine might be done in several circumstances. The amount of pee still in the bladder after voiding is measured with this test.
- High PVR levels may indicate dysfunctional bladder function and reflect inadequate bladder emptying.
Further tests
- Additional testing might be advised in some cases to evaluate bladder function and rule out other diseases.
- These may include imaging tests like ultrasound, cystoscopy, urography, and urodynamic testing, which evaluates bladder pressure and function during filling and emptying.1Diagnosis| Researched based study from Nlm.nih.gov ,2Diagnosis| Researched based study from Nlm.nih.gov
Treatment
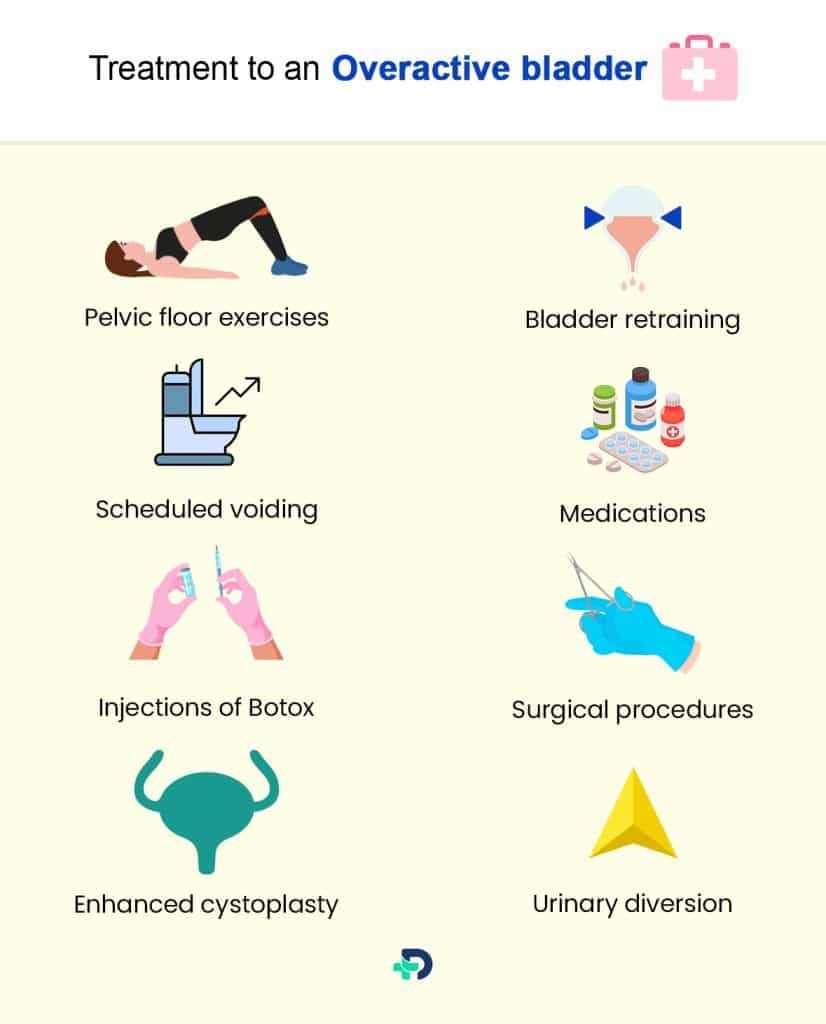
Treatment of an Overactive bladder
Behavioral techniques
It includes following:
Pelvic floor exercises
- Through exercises like Kegels, the pelvic floor muscles can be strengthened, enhancing bladder control and lowering urgency and leaks.
Bladder retraining
- This includes gradually extending the duration between voiding to increase bladder capacity and lessen urgency.
- This can help teach the bladder to hold more significant amounts of pee and reduce the frequency of urination by gradually lengthening the duration between bathroom trips.
Scheduled voiding
- You can manage the symptoms by emptying the bladder regularly and at predetermined intervals.
Medications
Following are the categories of medicines used to treat overactive bladder:
Anticholinergic medications
- These drugs, including oxybutynin, tolterodine, or solifenacin, aid in bladder muscle relaxation and lessen urine urgency and frequency. Constipation and a dry mouth are potential side effects.
Agonists of beta-3
- By activating beta-3 adrenergic receptors, the mirabegron relaxes the bladder muscle, increasing bladder capacity.
Neuromodulators
Neuromodulators techniques to manage overactive bladder are:
Stimulates the sacral nerve
- The sacral nerves, which regulate bladder function, are produced by electrical impulses provided by a device.
- This can improve bladder control by modulating nerve signals. People who don’t respond to previous treatments usually utilize it.
Tibia nerve stimulation using a needle
- The tibial nerve in the ankle is stimulated electrically by placing a small needle next to it to improve bladder function.
Injections of Botox
- By temporarily paralyzing the bladder muscle, botulinum toxin injections can minimize over activity.
- People who have not responded to other treatments are often the only ones who receive this treatment.
Surgical procedures
overactive bladder can also get treated by using one of the following surgical methods depends on the the severity of issue:
Enhanced cystoplasty
- A problematic situation where the bladder cannot hold enough urine may warrant consideration of an augmentation cystoplasty. This procedure uses a portion of the intestine to increase the bladder’s capacity.
Urinary diversion
- Rarely, when other therapies are unsuccessful, a surgical procedure may be carried out to divert urine away from the bladder. Typically, this is done by creating a hole in the bladder.1Treatment| Researched based study from Nlm.nih.gov ,2Treatment| Researched based study from Nlm.nih.gov
Diet
Dietary suggestions to manage Overactive bladder
Fluid intake control
- It’s crucial to stay hydrated, but instead of drinking a lot of liquids all at once, spread it out throughout the day.
- Drinking less water in the evening may also help you make fewer night-long trips to the loo.
Decrease of caffeine
- Caffeine is a diuretic, it might irritate the bladder and cause more pee to be produced. Think about cutting back on or quitting caffeinated drinks like coffee, tea, soda, and energy drinks.
Drinking in moderation
- Since it may have a diuretic impact, alcohol consumption should be restricted.
Acidic and spicy foods
- Spicy foods and foods high in acid (such as citrus fruits, tomatoes, and vinegar) may make some people’s bladder symptoms worse.
- Pay attention to your triggers and limit or avoid eating these things.
Optimum diet
- Always make an effort to consume a varied diet of fruits, vegetables, complete grains, and lean proteins.3Diet| Researched based study from Nhs.uk
Duration
How long does an Overactive bladder last?
The time frame can change depending on the underlying reason and particular conditions. Remembering that this chronic illness usually calls for continuing therapy rather than having a set duration.
Some lifestyle changes, behavioral therapy, and medications may subside the symptoms. Although the symptoms might be controlled and diminished, they might not entirely go.3Duration| Researched based study from Nlm.nih.gov
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
National Library of Medicine
Overactive Bladder Syndrome: Evaluation and Management | Diagnosis | Treatment
-
National Library of Medicine
Update on the management of overactive bladder | Diagnosis | Treatment
-
National Library of Medicine
Overactive bladder | Causes | Symptoms
-
National Library of Medicine
The overactive bladder | Causes | Symptoms
-
National Health Service
10 ways to stop leaks-Urinary incontinence | Diet