What is Osteoarthritis: Symptoms and Treatment

- Osteoarthritis
- 17 Aug 2023
Overview
What is Osteoarthritis?
Osteoarthritis or OA, is the most common type of arthritis. There are also many who refer to it as “wear and tear” arthritis or degenerative joint disorder. The palms, hips, and knees are the most common regions where this disease can be found1Overview| Researched based study from Cdc.gov
When a person has OA, the cartilage that is found within a joint will start to deteriorate, and the bone that is found underneath will start to change. These changes typically start out mild and gradually become more severe over time. Pain, stiffness, and edema are all possible symptoms of OA. In some situations, it can also cause impaired function and impairment, to the point that some people are no longer able to carry out their regular activities or hold down a job.

Symptoms
Osteoarthritis signs and symptoms
Osteoarthritis is a degenerative joint disease that often starts in one or a few joints and progresses slowly over time.
The following is a list of the common symptoms of osteoarthritis:
- Experiencing pain when using the joint, which may become better after taking some time off.
- For some people, the pain may be more severe during the nighttime hours when they are in the final phases of the disease. It’s possible for the pain to be localized or broad.
- Stiffness in the joints, which typically lasts for less than half an hour and occurs first thing when you wake up or after a span of resting.
- Alterations to the joints that might restrict joint movement.
- Swelling within and around the joint, particularly after engaging in a significant amount of exercise or making extensive use of that area.
- Alterations in the degree to which the joint can be moved.
- Having the sensation that the joint is unstable or loose.3Symptoms| Researched based study from Niams.nih.gov
The symptoms of osteoarthritis can have a variety of effects on joints. For instance:
Hands
- Bony enlargements and form changes in the joints of the finger can occur throughout the course of a person’s lifetime.
Knees
- There is a possibility that you will hear a grinding or scraping noise when you are walking or moving.
- Fatigue in the muscles and ligaments around the knee can, over time, cause the knee to buckle.
Hips
- There is a possibility that you will experience discomfort and stiffness in the hip joint, as well as in the groin, the inner thigh, or the buttocks.
- The discomfort that originates in the hip joint due to arthritis can occasionally travel all the way down to the knees.
- It’s possible that, as time goes on, you won’t be able to move your hip quite as far as you once could.
Spine
- You might experience stiffness as well as pain in the lower back or neck.
- Spinal stenosis is a condition that can occur in some persons as a result of natural changes in the spine.3Symptoms| Researched based study from Niams.nih.gov
As your symptoms continue to develop over time, it will become increasingly difficult for you to engage in tasks that you were previously able to do. Some examples of these activities include stepping up, sitting and getting up from a chair, holding a pan, and walking across a short distance. You may have feelings of exhaustion, difficulty sleeping, and depression as a result of the pain and other symptoms associated with osteoarthritis.
Causes
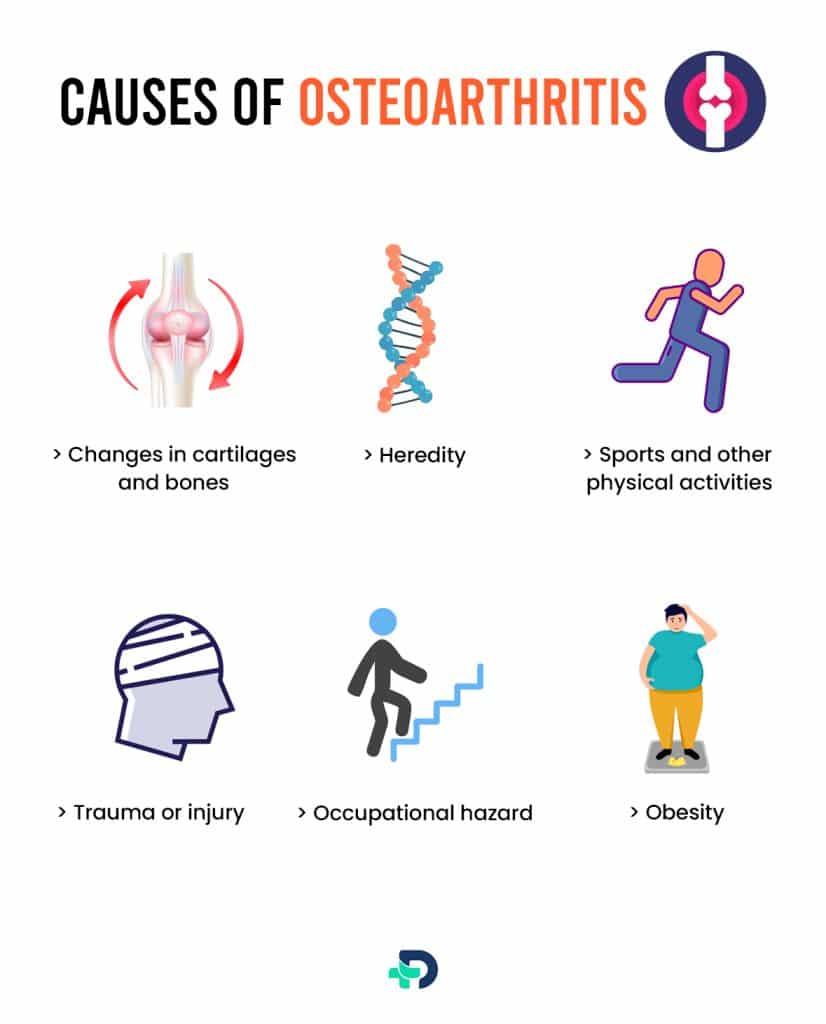
Causes of Osteoarthritis
Causes of Osteoarthritis can be one of the following:
- Changes in the structure of cartilages and bones
- Heredity
- Obesity
- Occupational hazards
- Injuries
- Any chronic disease
Changes in cartilages and bones
- Cartilage is a tough, rubbery tissue that cushions the ends of your bones where they connect together at joints. When the cartilage starts to break down and wear off, the pieces of the cartilage or the bones start to produce friction against the other’s surface. OA symptoms like pain, edema, and stiffness are frequently caused by this.
- As osteoarthritis progresses, bony spurs or more bone may develop around the impacted joint. There is a possibility that the ligaments and muscles that surround the joint will grow weaker and more rigid5Causes| Researched based study from Medlineplus.gov
Heredity
- In most cases, OA is passed down through families.
Obesity
- Being overweight raises the odds of developing osteoarthritis in the joints of the hip, knee, ankle, and foot. This is due to the fact that additional weight results in increased levels of wear and tear.
Trauma or injury
- Fractures and other types of joint traumas can put a person at a higher likelihood of developing OA in later life. Traumatic events affecting the cartilage and ligaments in your joints are also included in this category.
Occupational hazard
- Occupations that require crouching, kneeling, or lifting for more than an hour each day, as well as those that include ascending stairs or walking, all raise the risk for osteoarthritis (OA).
Sports and other physical activities
- Playing activities that require twisting of the body (like basketball or soccer), direct impact on the joint (like football), or throwing also raises the chance of developing osteoarthritis (OA).5Causes| Researched based study from Medlineplus.gov
Diseases that can cause osteoarthritis (OA) symptoms are
- Abnormalities of coagulation that lead to bleeding in the joints, such as hemophilia and thrombocytopenia
- Avascular necrosis refers to a group of conditions that cause the death of bone by cutting off blood flow to a joint.
- Other types of arthritis, including pseudo gout, rheumatoid arthritis, and long-term (chronic) gout
Risk factors
What are the risk factors for Osteoarthritis (OA)?
Factors which may increase the chances of getting OA are:
- Injury of the joint
- Aging
- obesity
- Gender
- Family history
Injury or overuse of a joint
- Injury or overuse of a joint, such as repeatedly bending a knee or placing stress on a joint in a repetitive manner, can cause damage to a joint and raise the risk of osteoarthritis in that joint.1Risk factors| Researched based study from Cdc.gov
Age
- The chances of getting diagnosed with OA rise with advancing years.
Gender
- After the age of 50, women have a higher chance of developing osteoarthritis (OA) than males do.
Obesity
- Obesity places additional strain on one’s joints, particularly those that are responsible for weight-bearing, such as the knees and hips.
- This stress raises the likelihood of developing osteoarthritis in that joint.
- In addition, obesity may have metabolic implications that raise the incidence of osteoarthritis (OA).1Risk factors| Researched based study from Cdc.gov
Genetics
- Individuals who come from families with a history of OA are at greater danger of developing the condition themselves.
- People who have osteoarthritis of the hand have a higher risk of developing knee osteoarthritis.
- Because of their race, some Asian populations have a lesser likelihood of developing OA.
Diagnosis
Diagnosis of Osteoarthritis
Conduct a thorough review of your medical history.
Your physician will be interested in knowing:
- Whether or not the joint has been harmed in the past.
- When the discomfort in the joints first started
- In what way does the pain manifest itself? Does it stay unwavering and unaltered or does it differ?
- Does it manifest itself in other locations in the body as well?
- Does it produce symptoms that occur at night?
- Does it only happen when you’re active or does it also happen when you’re at rest?
- Is there anything that can be done to alleviate the discomfort?4Diagnosis| Researched based study from Aaos.org
An examination of the body
The injured joint will then be examined by your doctor in a variety of positions to determine whether or not there is pain or restricted motion. They are going to search for:
- Crepitus refers to the cracking or grinding sounds that can be heard when bones rub against one another.
- Atrophy, or wasting away of muscle
- Indications that the problem may impact other joints
- Symptoms indicate damage to the muscles, tendons, and ligaments of the body
X-rays
In order to determine the severity of joint degeneration, x-rays are obtained in a variety of positions, including the following:
- Reduction in available joint space
- Bone that has been worn down or eroded.
- Spurs on the bones or other kinds of deformities
- In addition, X-rays can assist your doctor in differentiating between the various types of arthritis.4Diagnosis| Researched based study from Aaos.org
Laboratory Examinations
- Laboratory studies, such as blood testing, can sometimes be helpful in ruling out other diseases that cause symptoms that are similar to those caused by osteoarthritis4Diagnosis| Researched based study from Aaos.org
Treatment
Treatment of Osteoarthritis
There is currently no cure for OA; however, pain relief can be achieved by the use of medicine, assistive devices, and alternative treatments that do not entail the use of narcotics. When all other options have been exhausted, it may be possible to surgically fuse a broken joint or replace it with a new one that is constructed out of a medley of metal, plastic, and/or ceramic2Treatment| Researched based study from Arthritis.org
Medications
Medicines that relieve pain and inflammation caused by osteoarthritis can be taken in the form of pills, syrups, patches, gels, lotions, or injections. They are as follows:2Treatment| Researched based study from Arthritis.org
Analgesics
- Acetaminophen and opioids are two types of pain medications that fall under this category.
- Acetaminophen can be purchased nonprescription, but opioids require a prescription from a medical examiner.
NSAIDs (nonsteroidal anti-inflammatory drugs)
- These are the medications that are most frequently prescribed to treat pain and inflammation.
- These include aspirin, ibuprofen, naproxen, and celecoxib, all of which can be purchased without a prescription or over the counter.
Counterirritants
- These over-the-counter medications contain substances like capsaicin, menthol, and lidocaine that affect nerve endings. As a result, the painful area will feel cold, heated, or itchy in order to divert attention away from the true source of the pain.
Corticosteroids
- These anti-inflammatory prescription medications function in a manner that is analogous to that of a hormone known as cortisol.
- The medication can either be given orally or injected directly into the affected joint in a medical facility.
Platelet-rich plasma (PRP)
- This medicine is meant to assist reduce pain and inflammation, and it can be obtained from a doctor in the form of an injection.
Other medicines
- Oral drugs that have been approved by the FDA to treat osteoarthritis pain include the antidepressant duloxetine (Cymbalta), as well as the anti-seizure drug pregabalin (Lyrica).
Alternative therapies
It include:
Exercise
A good workout regimen to combat the pain and stiffness of OA consists of the following four components:
- Strength training helps to build muscle around sore joints, which in turn helps to relieve the tension that is placed on those joints.
- Stretching and other exercises that increase range of motion are helpful for reducing joint stiffness and keeping joints mobile.
- Aerobic exercise, also known as cardio, is beneficial for enhancing stamina and energy levels as well as reducing extra weight.
- Exercises that focus on balance can help prevent falls by strengthening the tiny muscles that are found around the knees and ankles.
Before beginning a new fitness regimen, it is important to receive advise and treatment from a medical examiner or a physical therapist.
Weight Loss
- Extra weight causes additional torque and stress on weight-bearing joints, such as those in the hips, knees, ankles, foot, and back; also, fat cells contribute to the production of inflammation.
- Shedding additional pounds can help ease joint pain and lessen the rate of joint degeneration.
- When one loses just one pound of weight, one relieves the joints of the lower body of the equivalent of four pounds of pressure.
Physiotherapeutic Treatments
Chiropractors, physical therapists, and occupational therapists are all capable of providing the following services:
- Exercises designed specifically to help you strengthen your joints and reduce joint pain.
- Details on the various natural treatments and products that are available to alleviate pain.
- Instructions to facilitate simpler movement while also protecting the joints.
- Devices like braces and shoe inserts, together with other supportive tools.
Surgery
- Surgical treatment of the joint can reduce pain and enhance function.
- During joint replacement surgery, diseased joints are surgically replaced with new ones in order to restore mobility and alleviate discomfort.2Treatment| Researched based study from Arthritis.org
- Hips and knees are the joints that are substituted the most frequently.
- Depending on the extent of the injury to the joint, an orthopedic surgeon might recommend the most appropriate procedure.
Management
How to manage Osteoarthritis?
The Arthritis Program at the CDC suggests the use of these five self-management strategies for the treatment and management of arthritis and related symptoms.1Management| Researched based study from Cdc.gov
Learn self-management skills.
- Participating in a self-management education class can assist people who have arthritis or other chronic disorders, such as OA, to understand how the condition affects their lives and boost their confidence in their ability to control their symptoms and live a healthy life.
Get some exercise and stay active.
- Physical exercise of at least moderate intensity should be performed for at least 150 minutes per week by adults, as recommended by experts.
- Every second spent being active is valuable, and even the smallest amount of action is preferable to doing nothing at all.
- Walking, swimming, and riding are examples of activities that have a moderate level of impact yet are nevertheless recommended.
- Participating in regular physical activity can lower one’s risk of getting other chronic diseases as well, including heart disease, stroke, and diabetes, amongst others.
Talk to your doctor.
- You can take an active role in managing your arthritis by keeping all of your scheduled appointments with your primary care physician and strictly adhering to the treatment plan that they have advised for you.
- This is of utmost significance if you also suffer from additional chronic diseases, such as diabetes or cardiovascular disease.
Keep your joints secure
- Trauma to the joints can either cause arthritis or make the condition worse.
- Pick exercises that are gentler on your joints, such as walking, cycling, or swimming.1Management| Researched based study from Cdc.gov
- These low-impact activities pose a low risk of injury because they do not include any twisting motions or excessive pressure being placed on the joints.
Takeaway
Takeaway tips
The most prevalent type of arthritis found in those over the age of 65 is osteoarthritis. In addition, it is one of the leading contributors to adults’ rates of physical impairment.
Osteoarthritis is a degenerative joint condition that occurs when the tissues that protects the ends of the bones within the joints gradually wear away over time. This leads to the bones rubbing against each other, causing pain and discomfort. These alterations typically manifest gradually and intensify with time, causing discomfort, stiffness, and swelling in the affected area. People who are afflicted with this disease may, in certain instances, lose the ability to hold down a job or carry out routine activities.
Although there is no cure for osteoarthritis, its symptoms can typically be managed with a combination of lifestyle modifications and medicine.
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
Centers for Disease Control and Prevention
Osteoarthritis (OA) | Overview | Risk factors | Management
-
Arthritis Foundation
Osteoarthritis | Treatment
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases
Osteoarthritis | Symptoms
-
American Academy of Orthopaedic Surgeons
Osteoarthritis | Diagnosis
-
Medline Plus
Osteoarthritis | Causes