Understanding Glaucoma: Types, Symptoms, Treatment and Prevention

- Glaucoma
- 22 Aug 2023
Overview
What is Glaucoma?
Glaucoma is a compilation of eye diseases. It is a disease that slowly and gradually damages the optic nerve. Glaucoma can lead to vision loss due to the degeneration of nerve tissue.
Glaucoma is commonly referred to as the “silent poison of sight” due to its ability to be asymptomatic and painless until significant vision impairment becomes clear.
Glaucoma is a prominent cause of blindness in people of 60 years and above. Early treatment can prevent blindness caused by glaucoma.
Causes
How does Glaucoma happen?
The eyes contain a fluid known as aqueous humor, which is responsible for the shape of eyes. In a healthy eye, there is adequate filtration of fluid.
- Fluid flow can sometimes be hampered during the outflow process. Excessive accumulation of fluid within the eye leads to an elevation in intraocular pressure (IOP).1Causes| Researched based study from Nlm.nih.gov
- Ocular hypertension refers to elevated eye pressure beyond the normal range. Individuals who have high intraocular pressure without any clinical signs of glaucoma are commonly referred to as suspects of glaucoma. This exerts force on the walls of the eye, resulting in destruction to the optic nerve.
- The optic nerve comprises over one million small nerve fibers. The degeneration of these nerve fibers leads to the emergence of visual blind spots and subsequent vision loss.
Prevalence
Prevalence
- The occurrence of open-angle glaucoma increases with age in individuals of European descent, with rates ranging from 0.4% at ages 40-44 to 2.7% at ages 70-74, and reaching 10.0% in individuals over the age of 90.
- Males are more prone than females.
- Congenital and juvenile glaucoma are uncommon conditions.4Prevalence| Researched based study from Nlm.nih.gov
Risk factors
Risk Factors
The chances of getting glaucoma may be increased by the following factors:
Age
- Individuals aged 60 and above have an increased risk to the disease. The incidence of glaucoma rises progressively with advancing age.
Race
- African Americans have a high risk of developing glaucoma compared to Caucasians, resulting in irreversible vision impairment.
Family history of glaucoma
- A positive genetic history of glaucoma 2Risk factors| Researched based study from Aoa.org is a potential risk factor for acquiring glaucoma.
Medical conditions
- Several doctors suggest that diabetes, cardiovascular disease and hypertension, may be linked with an increased risk of acquiring glaucoma.
Injury to the eye
- Severe trauma to the eye can lead to an immediate increase in intraocular pressure. Traumatic injuries like a sudden hit on the eyeball can lead to internal damage, leading to the closure of the drainage angle and then elevation of intraocular pressure.2Risk factors| Researched based study from Aoa.org
Use of corticosteroids
- Prolonged use of corticosteroids, such as cortisone, prednisone and hydrocortisone will increase the risk of secondary glaucoma in certain individuals.
Pseudo exfoliation syndrome
- Pseudo exfoliation syndrome is a frequent age-related generalized fibrotic tissue process that is important because it raises the risk of glaucoma.
Obstructive sleep apnea syndrome (OSA)
- It is a medical condition characterized by recurrent episodes of obstruction of the airway during sleep. Patients with obstructive sleep apnea syndrome have a 1.67-fold increased risk of developing glaucoma compared to individuals without this condition.
Other risk factors
- Thinner corneas
- Sensitivity of optic nerve
- Retinal detachment
- Tumors of the eye
- Inflammation of eyes
- Myopia2Risk factors| Researched based study from Aoa.org
Types
Types of Glaucoma
Glaucoma can be:
- Primary open angle glaucoma
- Angle-closure glaucoma
- Secondary glaucoma
- Normal tension glaucoma
- Congenital glaucoma
Primary open angle glaucoma
- It is one of the common forms of glaucoma. Optic nerve damage is painless and gradual and third vision loss occurs before it is noticed. It can also be due to an inefficient drainage system of the eyes, which builds up pressure in the eyes.
Angle-closure glaucoma
- It is less common but a medical emergency that causes sudden vision loss. This type of glaucoma is also known as narrow angle glaucoma or closed angle glaucoma. It occurs due to blockage in the drainage system of the eye. People with this glaucoma often have a narrow drainage angle causing sudden increase in the pressure of the eyes.
Secondary glaucoma
- This type of glaucoma happens because of injury to the eyes or any other eye disease. Possible causes include medication, trauma, medical conditions, cataract formation and abnormalities of the eye. The patient presents with rings or hallows around the lights, decreased field of vision and blurred vision etc.
Normal tension glaucoma
- In this type of glaucoma, the pressure in the eyes is optimal, but the optic nerve is still destructed. The reason is still not known. It can be due to a sensitive optic nerve.
Congenital glaucoma
- Kids who are born with a defect in the drainage angle will not allow the aqueous fluid to leave the eye normally. Common symptoms include cloudy corneas, sensitivity to light, and watery eyes.
Symptoms
Symptoms of Glaucoma
Open-angle glaucoma Symptoms
- Open-angle glaucoma usually lacks early warning signs or symptoms. The condition progresses gradually and may not result in noticeable visual impairment for an extended period of time.
- Individuals with open-angle glaucoma often remain asymptomatic and fail to detect any initial changes in their vision. This is primarily because the visual impairment affects the peripheral or side vision, while the sharpness or visual ability remains the same until the advanced stages of the disease.
- Vision loss is detected in patients when the disease has progressed and achieved an advanced stage. Treatment for glaucoma, including surgical interventions, does not have the ability to reverse vision loss caused by the condition.
Symptoms of acute angle-closure glaucoma
- Visual impairment characterized by a lack of clarity or sharpness in one’s vision.
- The phenomenon of observing rainbow-colored circles surrounding intense light sources.
- Intense pain in the eyes and head.
- Nausea or vomiting may be present alongside severe eye pain.
- Sudden onset of visual impairment.
Diagnosis
Diagnosis of Glaucoma
Glaucoma is diagnosed through eye examination. The diagnosis of glaucoma is confirmed by observing changes in the appearance of the optic nerve, loss of vision, loss of nerve tissue as the disease progresses over time.
Glaucoma testing encompasses:
- Get the patient’s medical history to identify symptoms, know general health conditions, and evaluate any relevant familial factors that may be causing the issue.
- Visual acuity measurements are done to assess the impact on vision.
- Tonometry is used to determine intraocular pressure. This diagnostic procedure is used to identify people with height risk of glaucoma. The standard intraocular pressure (IOP) should be less than 21 mmHg. Individuals with an intraocular pressure (IOP) exceeding 30 mmHg face a significantly elevated risk of vision loss resulting from glaucoma, which is approximately 40 times greater compared to those with an IOP of 15 mmHg or below.3Diagnosis| Researched based study from Nlm.nih.gov
- Pachymetry is used to know the thickness of the cornea. People with thinner corneas have a higher susceptibility to the development of glaucoma.
- Visual field testing, known as perimetry, is used to know potential impairment of the field of vision caused by glaucoma. This test assesses both peripheral and central vision by measuring the minimum detectable amount of light in different areas of vision.
- Retinal evaluation, involving the use of photos or scans of the optic nerve, is done to monitor temporal changes.
- Additional testing, such as gonioscopy, may be conducted. This procedure provides an examination of the angle anatomy, which is the site of ocular fluid drainage.
- Serial tonometry is a potential diagnostic test. This procedure involves obtaining multiple pressure measurements at different time points to monitor fluctuations in intraocular pressure all through the day.
- Furthermore, devices can be utilized for determining the thickness of nerve fibre and detecting tissue loss in specific areas of the nerve fiber layer.3Diagnosis| Researched based study from Nlm.nih.gov
Treatment
Glaucoma Treatment
The recommended target pressures for glaucoma are < 21 mm Hg for early stage, < 18 mm Hg for moderate stage, and < 15 mm Hg for advanced stage. Regardless of the specific target, regular monitoring of intraocular pressure is necessary to assess whether the disease has stabilized or progressed.
Medications
Prostaglandin analogs
- Prostaglandin analogs like Latanoprost and Bimatoprost are commonly prescribed as the initial topical treatment and are administered once daily, in the evening. They increase the trabecular and uveoscleral outflow, resulting in a fall of intraocular pressure.5Treatment| Researched based study from Nlm.nih.gov
Beta blockers
- Usually administered twice daily, these medications like Timolol maleate reduces the intraocular pressure by reducing the production of aqueous humor. The primary local adverse effect is the development of dry eye disease.5Treatment| Researched based study from Nlm.nih.gov
Alpha 2 adrenergic agonists
- Alpha 2 adrenergic agonists like Brimonidine will reduce aqueous humor secretion and increase uveoscleral outflow. Alpha 2 adrenergic agonists must not be topically given to children under the age of 12.
Carbonic anhydrase inhibitors
- Topical Carbonic anhydrase inhibitors like dorzolamide and brinzolamide will decrease the synthesis of aqueous humor.
Surgery
If the medications do not show any effect, then operative interventions can be utilized. The procedures for treating conditions include laser treatment that creates a drainage flap. By inserting a drainage valve, the fluid producing tissue can be destroyed. But surgery does not restore vision.5Treatment| Researched based study from Nlm.nih.gov
Laser surgery
- Laser trabeculoplasty is done to drain the eye fluid. It is performed in people who have open angle glaucoma. The ophthalmologist uses a laser to improve the drainage angle. This helps fluid flow out and fall in eye pressure.5Treatment| Researched based study from Nlm.nih.gov
Iridotomy
- It is done for people suffering from angle-closure glaucoma. The ophthalmologists will utilize a laser to make a minor hole in the iris. It will help in the flow of aqueous fluid to the drainage angle.
Trabeculectomy
- The ophthalmologist will make a small incision in the sclera. A small filtration lab is created, which absorbs the aqueous humor, and thereby reducing the pressure of the eyes.
Glaucoma drainage devices
- A drainage tube is implanted in the eye. The glaucoma drainage implant directs fluid to a reservoir. The reservoir is made under the conjunctiva. The fluid is then absorbed into blood vessels.
Cataract surgery
- By extracting the natural lens of the eyes, there will be lower eye pressure in people who have narrow angle glaucoma. The cataract surgery will increase the space for the aqueous fluid to exit, thus reducing the pressure in the eyes.
Prevention
Glaucoma Prevention
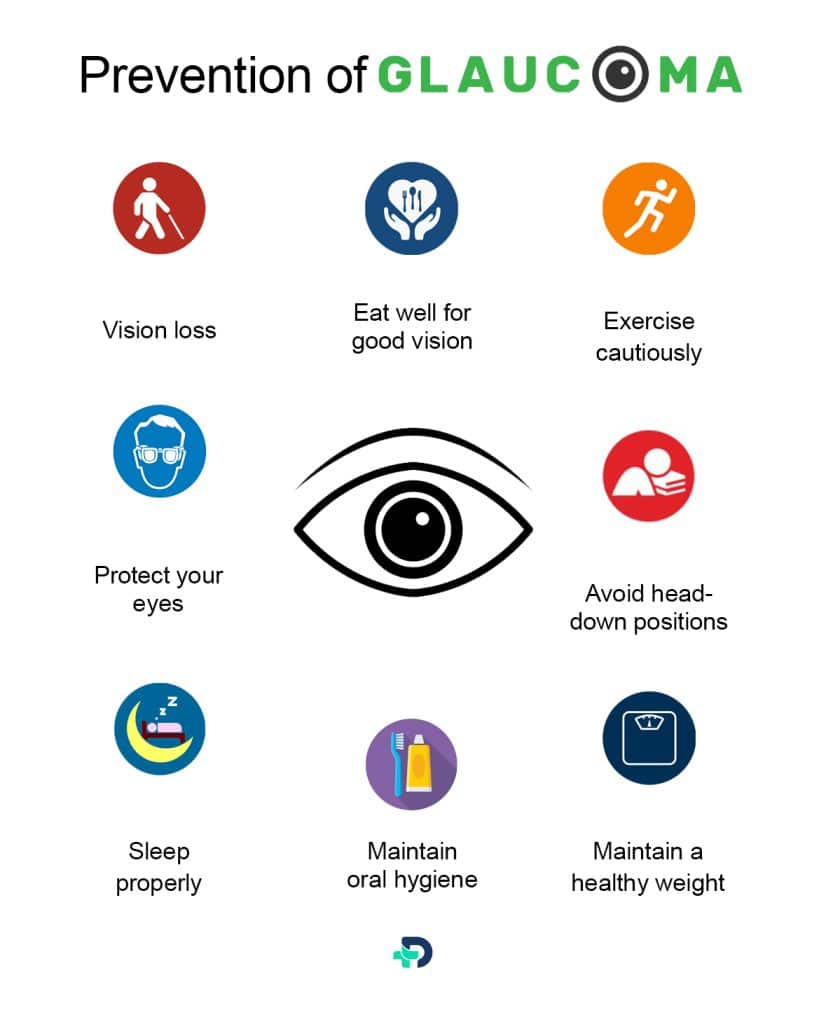
Glaucoma can be prevented by the following tips:
Catch the culprit of sight before vision loss
- You must Regularly see your ophthalmologist for appropriate eye exams if you are at risk for glaucoma. They can detect and treat the disease early. Use your glaucoma medications as prescribed by your doctor.
Consult your doctor if you are using steroids
- Long-term or high-dose steroid use can increase eye pressure, particularly for individuals with glaucoma. Oral or ocular steroids are highly prevalent to cause increase eye pressure.
Eat well for good vision
- Eat lots of leafy greens and colorful fruits and vegetables daily. They protect your body and eyes with vitamins and minerals. Eye-healthy foods are more effective than vitamins in preventing glaucoma.
Exercise cautiously
- Intense exercise can increase eye pressure. Brisk walking along with optimal regular exercise can lower eye pressure and improve overall health. Get a qualified trainer to teach you proper breathing techniques when lifting heavy weights.
Protect your eyes
- Wear protective eyewear during sports and when working at home or in the yard. Eye injuries can cause glaucoma.
Avoid head-down positions
- Avoid prolonged sittings of head-down positions if you have glaucoma or are at high risk. Avoid using inversion tables for back pain. Head-down positions increase eye pressure. Severe glaucoma patients should avoid specific yoga positions. Ask your doctor about avoiding a head-down position in your exercise routine.
Sleep properly
- Make sure that you don’t fall asleep with your eye facing towards the pillow or on your arm if you have glaucoma. OSA (obstructive sleep apnoea) increases glaucoma risk. Get tested for OSA if you snore heavily or stop breathing at night.
Wear sunglasses to shield your eyes from the sun
- UV rays of sunlight may cause glaucoma. You must wear polarized sunglasses and a hat outdoors.
Maintain oral hygiene
- Gum disease is linked to damage to the optic nerve in glaucoma. Maintain daily oral hygiene and visit your dentist regularly.
Get your blood sugar levels checked
- There is evidence that the development of glaucoma may be influenced by insulin resistance. Elevated blood sugar levels are associated with increased intraocular pressure, a known risk factor for the development of glaucoma.
Maintain a healthy weight
- High BMI increases eye pressure, while low BMI increases the risk of primary angle glaucoma due to low brain pressure pushing the optic nerve inward. So, Aim for a moderate weight, not too little or too much.
Tell your ophthalmologist if you are on any hypertensive medications
- When Blood pressure falls down during sleep , it can lead to glaucoma. Inform your ophthalmologist if you take blood pressure medication at night or experience low blood pressure symptoms. Discuss with your primary care doctor. Do not alter your blood pressure medication without medical guidance.
Dietary Suggestions
Reduce your risk of Glaucoma by following Dietary modifications
Food needs to avoid:
To reduce the risks linked to glaucoma, it is advisable to avoid certain food items. Avoiding these items may lead to the improvement of eye health.
- It is advisable to limit salt intake to a moderate level, ideally minimizing it as much as possible.
- Coffee contains antioxidants, but excessive consumption may elevate blood pressure in individuals with glaucoma.
- Refrain from consuming food with high calorie content.
- Avoid consuming liquids in one sitting. Instead, drink fluids regularly.
Nutritious food choices for glaucoma prevention:
A diet rich in vitamins and nutrients contributes to improved health and the prevention of ailments. Many glaucoma patients wonder if diet changes can cure their condition. Diet modifications have the potential to prevent the development of glaucoma, but they do not possess curative properties for the condition.
Eat Carotenoid rich food
Consuming carotenoid-rich vegetables can significantly improve vision health.
- Kale
- Carrots
- Cabbage
- Green beans
- Cantaloupe
- Broccoli
- Sweet potato and radishes.
- Beets
- Sprouts
Add antioxidants
Oxidative stress is closely linked to optic nerve damage in glaucoma. A diet rich in antioxidants is recommended for the prevention of glaucoma, as it aids in protecting the eye from damage.
Here are some recommended sources of antioxidants that are beneficial to include in your daily dietary intake:
- Black and green tea
- Flax seeds
- Cranberries
- Spinach and acai berries
- Pomegranate
- Dark chocolate
Take Dairy products
- Consuming sufficient amounts of dairy products, such as milk and cheese, is important for promoting and potentially preventing eye-related conditions.
Ginkgo Supplements
- Ginkgo Biloba Supplements were found to be effective in reducing oxidative stress and promoting retinal blood flow.6Dietary suggestions| Researched based study from Nlm.nih.gov
Outlook
The Outlook
Successful treatment of glaucoma requires mutual efforts between you and your healthcare providers. The glaucoma treatment will be given by your ophthalmologist. It is your responsibility to adhere to the instructions provided by the doctor and utilize the prescribed eye drops.
Quick detection, prompt treatment, and regular monitoring are essential for managing glaucoma and minimizing the risk of vision impairment.
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
National Library of Medicine
Glaucoma | Causes
-
AMERICAN OPTOMETRIC ASSOCIATION
Glaucoma | Risk Factors
-
National Library of Medicine
The Diagnosis and Treatment of Glaucoma | Diagnosis
-
National Library of Medicine
Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis | Prevalence
-
National Library of Medicine
The Diagnosis and Treatment of Glaucoma | Treatment
-
National Library of Medicine
The Role of Diet in Glaucoma: A Review of the Current Evidence | Dietary Suggestions