Gastroparesis Life Expectancy, Risks, Causes & Management

- Stomach
- 29 Sep 2023
Introduction
Gastroparesis
The typical action of the muscles of the stomach is hampered by gastroparesis. Simply put, it occurs when the stomach does not adequately evacuate its contents. Normally, after eating, your stomach muscles contract to aid in the breakdown of the meal and move it into the small intestine for additional digestion. However, these contractions are attenuated or don’t occur adequately in persons with gastroparesis.

- Gastroparesis 1 Introduction | Researched based study from National Institutes of Health can develop for a variety of reasons, including pre existing conditions like diabetes, drugs, and previous surgery.
- Consult a healthcare provider for an accurate diagnosis and advice if you think you may have gastroparesis or are experiencing symptoms.
Who is at the risk of developing Gastroparesis?
In the case of gastroparesis, the stomach’s ability to empty its contents takes longer than usual, resulting in symptoms including nausea, vomiting, and bloating.
Causes
Potential Causes of Gastroparesis
Diabetes:
- High blood sugar levels can harm the nerves that govern the contraction and movement of food through the digestive tract in the stomach.
Intraoperative:
- The vagus nerve, which regulates stomach movement, can be damaged or disrupted during surgical procedures involving the stomach or adjacent organs.
Vagus Nerve Damage:
- The vagus nerve can be injured by conditions like Parkinson’s, multiple sclerosis, and autoimmune illnesses.
Medications:
- Some medicines, particularly those that have an effect on the neurological system, can cause gastroparesis by interfering with stomach contractions.
Viral Infections:
- Infections like herpes or the Epstein-Barr virus can inflame the stomach muscles’ nerves and harm them.
Hormonal Alterations:
- The stomach’s capacity to contract efficiently can be affected by changes in hormone levels.
- Conditions like hypothyroidism and excessive amounts of particular hormones are examples of this.
Eating Issues:
- Due to their inconsistent eating habits and behaviors, conditions like anorexia and bulimia can impair normal stomach function.
Scleroderma:
- This inflammatory condition can make tissues stiff and rigid, which might impair the stomach muscles and result in gastroparesis.
Disorders of the Smooth Muscles of the Digestive Tract:
- Amyloidosis is one condition that can cause the stomach to empty more slowly.
Idiopathic:
- When the precise origin of gastroparesis is unknown, it is referred to as idiopathic.
- The regular coordination of muscle contractions and nerve impulses that carry food through the digestive system might be hampered by these many factors.
- As a result, food remains in the stomach longer than it should, which causes the gastroparesis symptoms.
- It’s crucial to collaborate with medical experts to identify the underlying reason and create a suitable treatment strategy.
How hard is it to live with Gastroparesis?
It is a condition where the stomach muscles don’t work properly, leading to delayed emptying of food into the small intestine.
Symptoms
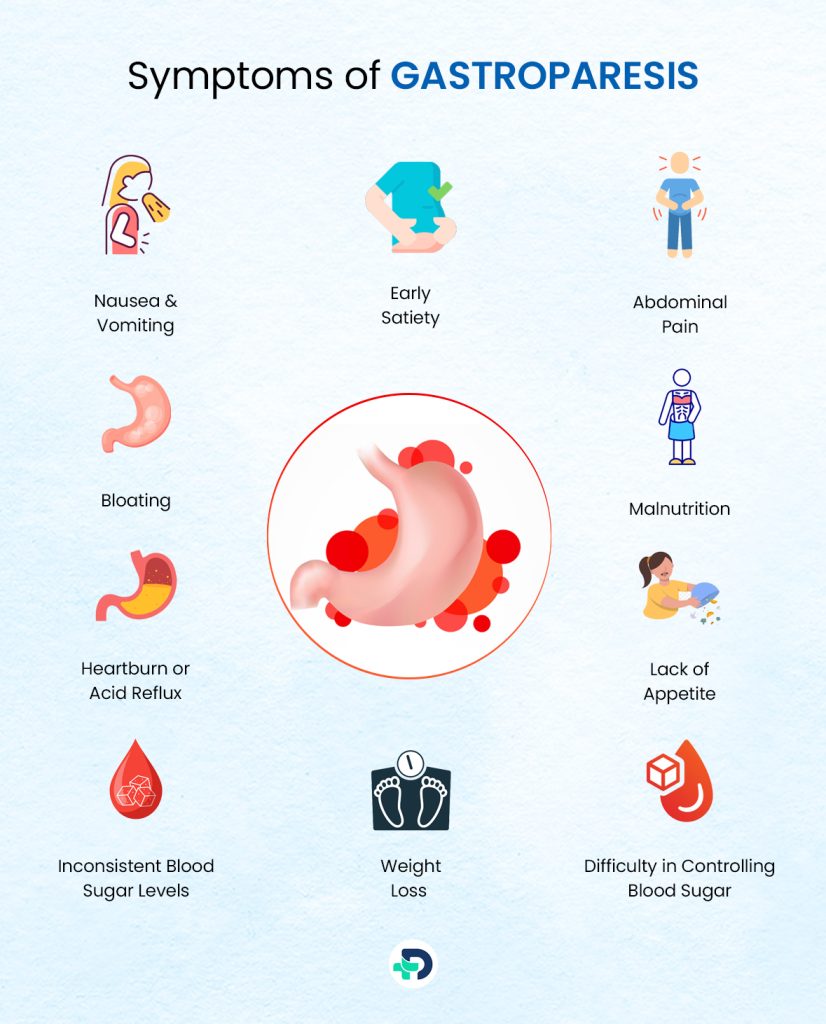
Symptoms of Gastroparesis : 2 Symptoms | Researched based study from National Institutes of Health
Nausea & Vomiting:
- Feeling queasy and puking up, especially after eating.
Early Satiety:
- Feeling full quickly, even after eating small amounts of food.
Bloating:
- Discomfort in the abdomen due to food staying in the stomach for longer periods.
- Aching or discomfort in the stomach area, which can range from mild to severe.
Heartburn or Acid Reflux:
- Backflow of stomach acid into the esophagus, causing a burning sensation.
Lack of Appetite:
- Reduced desire to eat due to persistent feelings of fullness or discomfort.
Unintended Weight Loss:
- Dropping pounds without trying, possibly due to reduced food intake.
Inconsistent Blood Sugar Levels:
- Fluctuations in blood sugar due to unpredictable digestion and nutrient absorption.
Malnutrition:
- Inadequate absorption of nutrients can lead to deficiencies and related health issues.
Difficulty in Controlling Blood Sugar:
- Especially problematic for individuals with diabetes, as delayed digestion affects glucose levels.
Feeling of Food Sitting in the Stomach:
- Sensation that food remains in the stomach long after eating.
If you’re experiencing these symptoms frequently, it’s essential to consult a healthcare professional. They can provide proper diagnosis and guidance on managing Gastroparesis to improve your quality of life.
Is Gastroparesis and GERD same?
- There exists a discernible distinction between gastritis and gastroesophageal reflux disease (GERD) in terms of the location of inflammation inside the gastrointestinal (GI) tract, despite the shared characteristic of inflammation.
- Gastritis is characterized by the presence of inflammation inside the gastric mucosa, namely in the stomach, whereas gastroesophageal reflux disease (GERD) involves inflammation within the esophagus.
Is Gastroparesis very serious?
- Even if it does not pose a threat to everyone’s life, it can have a substantial impact on quality of life.
- In severe circumstances, diabetics may experience issues like blood sugar swings or malnutrition.
- Dietary adjustments, medicines, and even surgical treatments are all part of the treatment.
- To avoid problems, it’s critical to manage symptoms and get medical help.
Diagnosis
Diagnosis of Gastroparesis
- In the case of gastroparesis, the stomach empties its contents more slowly than usual. It can be diagnosed using a few techniques 3 Diagnosis | Researched based study from National Institutes of Health .
Medical Background:
- Your symptoms, general health, and any drugs you’re taking will all be discussed with your doctor.
Physical Examination:
- A physical examination could be done to look for indications of bloating, discomfort, or weight loss.
Gastric Emptying Research:
- This test is important. A scanner will measure how quickly food you eat that contains a little bit of radioactive material leaves your stomach.
Breath Examination:
- When you drink a specific beverage and then blow into a bag, the gases measured can assist determine how efficiently your stomach is emptying.
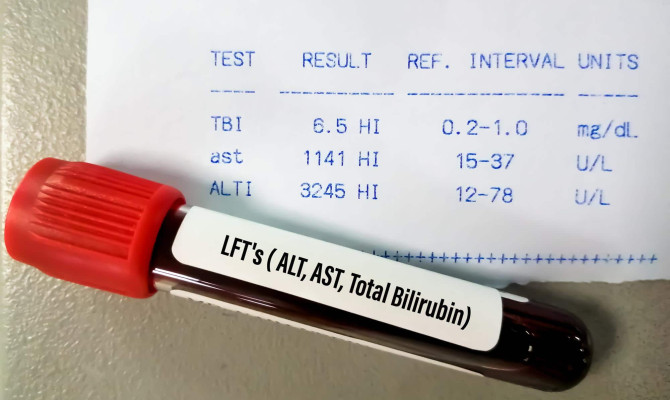
Blood Examinations:
- These can rule out further illnesses including diabetes or thyroid problems.
Upper Endoscopy:
- A little tube with a camera is put through your mouth to examine the lining of your stomach for any indications of gastroparesis.
Smart Pill:
- This pill has a tiny electronic device that you ingest to track how long it takes for the pill to pass through your stomach.
ElectroGastrography (EGG):
- Through electrodes applied to your skin, this captures the electrical activity of your stomach muscles.
Your doctor will assess whether you have gastroparesis based on these tests and your symptoms, and will then recommend the most suitable therapies.
Can blood tests detect Gastroparesis?
Urine and blood tests might be used by your doctor to diagnose gastroparesis. Urine tests are useful in detecting infections, dehydration, diabetes, and kidney issues. Blood testing can reveal inflammatory conditions, dehydration, malnutrition, and parasitic manifestations.
Impact
Impact of Gastroparesis on Life Expectancy:
Not all cases of gastroparesis result in symptoms or indicators. When they do, these symptoms are frequently present:
- Vomiting
- Nausea
- Acid reflux
- Stomach ache
- Bloating
- Decreased Appetite
- Gastroparesis impacts some people’s quality of life but is not a life-threatening condition.
- During flare-ups, they might not be able to finish specific tasks or work. However, some people deal with possibly fatal problems.
Diabetes:
- Gastroparesis can exacerbate diabetes because the gradual passage of food through the stomach and intestines might result in erratic variations in blood sugar levels.
- Blood sugar levels may decrease while food is still in the stomach and then rise once it reaches the bowels.
- The inability to regulate blood sugar as a result of these oscillations increases the risk of catastrophic issues like heart attack, stroke, and harm to essential organs.
Malnutrition and Dehydration:
- Dehydration that poses a life-threatening risk can result from persistent vomiting and gastroparesis.
- Additionally, because the illness interferes with the body’s ability to absorb nutrients, it can result in malnutrition, which has the potential to be fatal.
Obstruction:
- Some gastroparesis sufferers can get lumps in their stomachs from undigested food.
- These lumps, or bezoars,might obstruct the small intestines, albeit they are uncommon.
- Blockages might result in a dangerous illness if they are not immediately treated.
Adverse effect of cancer:
- Malignancy does not cause gastroparesis, however it might develop as a side effect of malignancy.
- After a cancer diagnosis, gastroparesis symptoms are frequently misdiagnosed as chemotherapy-induced nausea and vomiting or cancer cachexia.
Cancer cachexia:
- It is the term used to describe the weight loss and muscle loss experienced by people with advanced cancer.
- Pancreatic cancer and upper gastrointestinal (GI) tract tumors have both been linked to gastroparesis.
Is Gastroparesis permanent?
- It is not possible to treat gastroparesis. It is a persistent, long-lasting condition that cannot be cured.
- While there is no known treatment for this condition, your doctor can come up with a strategy to assist you manage your symptoms and lower the risk of major problems.
Complications
Complications of Gastroparesis
Malnourishment:
- The body may not get adequate nutrients as food sits in the stomach for a prolonged period of time, leading to shortages and weight loss.
Fluctuating Blood Sugar:
- People with diabetes may find it difficult to control their blood sugar levels due to gastroparesis.
Gastroesophageal Reflux Disease (GERD):
- Delayed stomach emptying can result in stomach acid leaking back into the esophagus, causing heartburn and other unpleasant symptoms.
Bacterial Expansion:
- Food that moves slowly can promote bacterial growth in the stomach, which can result in infections and digestive issues.
Nausea & Vomiting :
- Due to the buildup of uneaten food, gastroparesis frequently results in nausea and vomiting.
Dehydration:
- Consistent nausea and vomiting can prevent people from consuming enough fluids, which can result in dehydration.
Gastrointestinal Obstruction:
- Undigested food can harden and become solid masses that clog the digestive tract and cause excruciating discomfort.
Unpredictable Medication Absorption:
- Patients with gastroparesis may not regularly absorb their medications, which can reduce their efficacy.
Impaired Quality of Life:
- Prolonged symptoms including nausea, vomiting, and abdominal discomfort can seriously affect one’s ability to carry out everyday tasks and maintain emotional stability.
Electrolyte Imbalance:
- The body’s electrolyte balance can be upset by frequent vomiting and fluid loss, which can result in fatigue and other health problems.
Gastroparesis Flares:
- Periodically, symptoms can get worse, making it difficult to function in everyday life.
Aspiration Pneumonia:
- While vomiting, food particles and stomach acids may make their way into the lungs, where they may lead to lung infections.
Medication causing Delayed Stomach Emptying:
- Due to delayed stomach emptying, some drugs may not work as intended.
Impairment of Stomach Function:
- In severe situations, the illness may deteriorate as the stomach muscles weaken over time.
Changing one’s diet, taking drugs, and perhaps undergoing surgery are all part of managing gastroparesis. Working closely with medical professionals is crucial for preventing and treating these issues.
Is Gastroparesis cancerous?
- Gastroparesis is not a malignant condition.
- Your stomach muscles don’t function properly as a result of this medical problem, which causes poor digestion and a number of symptoms include nausea, vomiting, and a rapid increase in hunger.
- This occurs as a result of damaged nerves that regulate the stomach muscles.
- Contrarily, cancer entails the unchecked expansion of aberrant cells that have the potential to infiltrate surrounding tissues.
- Gastroparesis is a distinct condition that needs medical treatment to treat its symptoms and underlying causes; it is unrelated to cancer.
Management
Treatment for Gastroparesis:
Management entails food modifications, medication, and lifestyle changes.
Diet:
- Eating more frequently and in smaller portions can help symptoms subside. Put an emphasis on foods that are simple to digest, such as lean proteins, prepared veggies, and low-fiber alternatives.
- Foods high in fiber and fat should be avoided as they can impede digestion.
Medicines:
- Your doctor may recommend drugs to induce stomach contractions and manage symptoms.
- Drugs which increase gastric motility are popular choices, although they may have side effects and need to be carefully monitored.
Nutrition:
- Despite eating fewer meals, a qualified dietitian can help you make sure you’re getting enough nutrients.
- To aid in digestion, they might suggest liquid or pureed meals.
Blood sugar control:
- If you have diabetes, it’s important to keep your blood sugar levels under control.
- Changes can make gastroparesis symptoms worse.
Lifestyle Changes:
- To promote proper digestion, try to avoid reclining down after meals.
- After eating, some little exercise can also be beneficial.
Hydration:
- Drink little amounts of water frequently throughout the day to avoid dehydration since gastroparesis might make it difficult to consume a lot of liquids at once.
Prokinetic Drugs:
- These drugs can increase stomach contractions, which helps the stomach empty. Their efficiency varies from person to person nonetheless.
Antiemetic Drugs:
- If your nausea and vomiting are severe, your doctor may recommend drugs to treat them.
Surgical Options:
- If alternative therapies are ineffective, serious instances may warrant consideration of surgical operations.
- Options include pyloric surgery or gastric electrical stimulation which are discussed below in the article briefly.
Regular Follow-up:
- Keep in touch with your healthcare provider for routine checkups and modifications to your treatment plan.
Keep in mind that each patient’s treatment plan is unique. Find the best methods for controlling your gastroparesis by working together with your healthcare practitioner.
Does physical exercise help in Gastroparesis?
Physical activity is often one of the most effective symptom control techniques for gastroparesis. Intensity is important; if you work out too hard, their symptoms will certainly worsen. Aim for at least 30 minutes of light to moderate physical activity every day, such as walking, yoga, or cycling.
What is the best vitamin for Gastroparesis?
- Due to its impact on the digestive and absorptive processes, gastroparesis can lead to potential deficiencies in vital micronutrients, including vitamin B-12, iron, and calcium, among individuals affected by this condition. The utilization of a liquid vitamin and mineral supplement has the potential to deal with the deficiency of essential nutrients.
Surgery
Surgery as an Option for Gastroparesis
- Surgical therapies may be considered if other treatments, such as dietary changes, medications, and lifestyle modifications, are unsuccessful. A few surgical options 4 Treatment | Researched based study from National Institutes of Health are as follows:
Implanting a gastric stimulator:
- This entails implanting a tiny, pacemaker-like device under the abdomen’s skin.
- It provides the stomach muscles with electrical signals to control their contractions and enhance gastric emptying.
Pyloroplasty:
- The pylorus, or opening between the stomach and small intestine, is widened during this treatment.
- This may facilitate easier passage of food from the stomach into the intestines.
Gastric Bypass:
- In this more involved procedure, the stomach may be partially or completely removed.
- To enhance food transit and lower the size of the stomach, a partial gastrectomy may be performed in some circumstances.
Jejunostomy:
- Directly into the small intestine is placed a tube that is put through the abdominal wall.
- This enables food to enter the intestine without going via the stomach.
Feeding Tube:
- A feeding tube can be inserted directly into the stomach or small intestine in extreme circumstances where oral intake is not feasible.
- This guarantees that the body gets the nutrients and calories it needs.
Total Parenteral Nutrition (TPN):
- TPN 5 TPN | Researched based study from American College of Gastroenterology feeds nutrients directly into the bloodstream through a vein if the digestive tract cannot be used.
- When more practical alternatives cannot be used, this is frequently used.
- It’s crucial to remember that these operations carry dangers and could result in difficulties, despite the fact that they can provide comfort.
- Because every patient’s circumstances are different, the choice of intervention depends on things including the patient’s preferences, the degree of their gastroparesis, and their general health.
- Always seek the opinion of a licensed medical practitioner to get tailored guidance and choose the best course of action.
New advances for Gastroparesis
- Patients who have not responded to conventional treatments may have a specialised operation called G-POEM (gastric peroral endoscopic myotomy). Endoscopy is used to do minimally invasive surgery on the stomach.
- After receiving intravenous sedation, a test known as an endoscopy is carried out. The stomach is where the surgery takes place, and a tiny tube is put there.
- Your doctor may also go over other experimental possibilities with you, such as having an electric stimulation device surgically implanted on your stomach. The electrical stimulation aids with symptom control.
- There are a number of brand-new pharmaceuticals in development that show promise in treating gastroparesis.
Surgical Complications of Gastroparesis:
The inability of the stomach to evacuate its contents is known as gastroparesis. Surgery may be an option in extreme circumstances to relieve discomfort. However, difficulties can arise during operations.
Infection:
- Infection at the incision site or inside the abdomen is a possibility following surgery.
- To stop this, antibiotics are frequently administered.
Bleeding:
- Following surgery, there may be bleeding, either right away or a few days later.
- Additional medical care may be necessary in this situation.
Digestive Issues:
- Gastroparesis surgery might exacerbate digestive problems, resulting in nausea, vomiting, or diarrhea.
Injury to Nearby Organs:
- Accidental injury to nearby organs during surgery, such as the intestines or blood vessels, can result in additional difficulties.
Gastrointestinal outflow:
- Following surgery, the stomach’s link with the intestines may not repair properly, allowing stomach contents to seep into the abdomen.
Scar Tissue Formation:
- Scar tissue may develop internally during surgery, which could be painful and prevent food from moving normally.
Anesthesia Complications:
- During surgery, general anesthesia may result in respiratory issues, allergic responses, or other negative effects.
Slow Healing:
- Gastroparesis may prolong the time it takes for surgical incisions to heal by slowing down the healing process.
Nutritional Issues:
- Surgery may interfere with the body’s ability to absorb nutrients, resulting in a deficiency in vital vitamins and minerals.
- Before considering surgery for gastroparesis, it’s crucial to have a thorough discussion with the medical staff and to assess the potential benefits against these complications.
Remedies
Home Remedies for Gastroparesis
While there is no substitute for medical guidance, several home treatments may offer momentary relief:
Ginger:
- Ginger can aid in digestion improvement and nausea relief. Try drinking ginger tea or biting into a piece of ginger.
Smaller Meals:
- Eating smaller, more frequent meals can ease digestion by reducing the strain on your stomach.
Avoid High-Fiber and Fatty Foods:
- These foods can be more difficult to digest. Lean proteins and prepared veggies are good low-fiber choices.
Hydration:
- It’s crucial to maintain proper hydration. Drink water frequently throughout the day to stay hydrated.
Herbal Teas:
- Chamomile or peppermint tea may help reduce discomfort and calm your stomach.
Probiotics:
- Yogurt is a probiotic-rich food that can help digestion and support a healthy gut.
Physical Activity:
- Moderate exercise, such as walking, might improve digestion and lessen symptoms.
Avoid carbonated beverages:
- Because they can make you feel bloated and uncomfortable.
Reflux:
- If reflux is a concern, consider sleeping with your head slightly elevated.
Warm compress:
- Applying a warm compress to your stomach may help you feel better.
Remember that while these treatments may provide short-term solace, they cannot reverse gastroparesis. It’s crucial to speak with a medical expert for an accurate diagnosis and available treatments.
Quality of life
- When we discuss the quality of life in gastroparesis, we take into account how these symptoms impact everyday tasks, feelings, and general wellbeing. Imagine having random episodes of vomiting, feeling constantly sick, and being unable to eat without discomfort. Everything from going out to lunch with friends to producing work or academically might be affected by this.
- People who have gastroparesis may need to carefully manage their symptoms, adjust their diets, and take medications. These changes may have an impact on their capacity to engage in typical activities, mental health, and social life.
- Striking techniques to effectively control symptoms, asking for help from medical professionals, and striking a balance that enables a fulfilling existence despite the difficulties caused by the condition are all important components of maintaining a high quality of life in gastroparesis.
Conclusion
Gastroparesis Life Expectancy – Follow Medical Advices
Understanding how gastroparesis affects life expectancy highlights the significance of early detection, proactive management, and lifestyle modifications.
Although gastroparesis might result in consequences, each person’s prognosis is unique.
Many people can maintain a respectable quality of life with appropriate medical care, dietary changes, and symptom management.
The life expectancy of people with gastroparesis can be increased by maintaining regular contact with medical professionals, adhering to prescribed treatments, and putting an emphasis on general wellbeing.
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
National Institutes of Health
Introduction
-
National Institutes of Health
Symptoms
-
National Institutes of Health
Diagnosis
-
National Institutes of Health
Treatment
-
American College of Gastroenterology
TPN