Acute pancreatitis : Complications and Management

- Acute pancreatitis
- 14 Aug 2023
Overview
What is Acute pancreatitis ?
Acute pancreatitis refers to a medical condition that causes a sudden inflammation (swelling) of the pancreas. It can range greatly in severity, from mild illnesses that just require conservative care to severe and complex disorders with substantial morbidity and mortality.
A long, flat gland in the upper belly, the pancreas is located behind the stomach. It creates hormones and enzymes for digestion, which control, among other things, how the body uses glucose. Any inflammation of this pancreas is called pancreatitis. It can be acute, in which case short-term inflammation appears quickly, or chronic, in which case it persists or recurs. 1What is Acute pancreatitis ? | Researched based study from nih.gov Globally, there are 34 cases of acute pancreatitis per 100,000 persons each year. In the United States, pancreatitis contributes significantly to morbidity and healthcare costs. 2What is Acute pancreatitis ? | Researched based study from nih.gov A few milder instances recover on their own, but severe cases must be treated to avoid potentially fatal consequences.

Causes
Causes of Acute pancreatitis
- Gallstones are the most frequent reason. 3Causes of Acute pancreatitis | Researched based study from nih.gov
- Elevated blood fat (triglyceride) levels
- A few drugs
- A rise in alcohol consumption
- Pancreas injury caused by trauma
- Bacterial illnesses, including leptospirosis, tuberculosis
- Viral infections, such as hepatitis, measles, and HIV
- Certain parasite illnesses
- Autoimmune disorders that cause pancreatitis
- An elevated blood calcium level
- Particular genetic changes
- Kidney failure
- Organophosphate poisoning and scorpion bites
- Smoking 4Causes of Acute pancreatitis | Researched based study from nih.gov
Symptoms
Symptoms of Acute pancreatitis
Acute pancreatitis typically begins with discomfort in the upper abdomen, which may come on gradually or quickly, occasionally move to the back, range from mild to severe, and linger for many days
- Abdominal pain is the primary symptom, which can range in intensity
- An abdomen that is swollen and painful
- Fever
- Vomiting and nausea
- Rapid heartbeat
- Rapid, shallow breathing
- A breathing problem
- Confusion
- Jaundice (mild)
Prevention
Prevention of Acute pancreatitis
To some extent, the following steps might prevent acute pancreatitis:
- Give up or cut back on alcohol use 5Prevention of Acute pancreatitis| Researched based study from nih.gov
- Engage in regular exercise
- Stop smoking
- Continue to be a healthy weight
- Have a well-balanced diet that is high in fruits and vegetables
- Refrain from consuming fatty foods that are high in cholesterol
- Increase your dietary fiber intake 6Prevention of Acute pancreatitis | Researched based study from nih.gov
- Beware of medications known to cause acute pancreatitis
Diagnosis
How to diagnose Acute pancreatitis ?
A pancreatitis diagnosis comprises questioning about symptoms, a medical history, a physical examination, and a few tests to confirm the diagnosis:
- Blood and urine test – to check for elevated white blood cell count, kidney function, and liver enzyme level, as well as high concentrations of pancreatic enzymes including amylase and lipase
- Ultrasound – for finding gallstones and other blockages
- Computed tomography (CT) – to detect gallstones and determine the severity of pancreatic inflammation
- Magnetic resonance imaging (MRI) – to look for any abnormalities in the gallbladder, pancreas, or ducts
- An endoscopy – to view the anatomy of the pancreas in detail, including any cysts, ruptures, blockages, or narrowing
Complications
Complications associated with Acute pancreatitis
There are a few serious complications of acute pancreatitis, as follows:
- Pseudocysts – formed when pancreatic secretions gather together outside of the body’s ductal system
- Pancreatic necrosis – is a consequence that poses a serious risk to life. A pancreas infection may result in a lack of blood flow, which causes the cells to die. As a result, additional bacteria are attracted to the area, and the infection can begin to spread
- Septicemia – this emergency occurs when the infection has entered the blood
- Septic shock – occurs when the body mounts a defense against an infection that has spread to the bloodstream. The blood vessels may widen as a result of this immunological response, causing the blood pressure to drop (septic shock)
- Multiple organ failure – Septic shock, which reduces blood flow to important organs, can fail several organs
- Pulmonary involvement – A significant fluid buildup could squeeze the lungs and cause respiratory distress syndrome
- Other hazards include gastrointestinal bleeding and kidney failure
- Chronic pancreatitis – recurring acute episodes caused by gallstones, can develop into chronic pancreatitis (CP), a dangerous disorder that can have a negative influence on one’s quality of life 7Complications associated with acute pancreatitis| Researched based study from ist.psu.edu and result in major long-term problems
- Diabetes – Those with pancreatitis have a more than two-fold increased lifetime risk of getting new-onset diabetes compared to people in the general population who have never had pancreatitis.5Complications associated with acute pancreatitis| Researched based study from nih.gov
- Pancreatic cancer – In some cases, chronic pancreatitis can lead to pancreatic cancer
- Mortality due to complications like multiple organ failure in cases of severe acute pancreatitis
Management
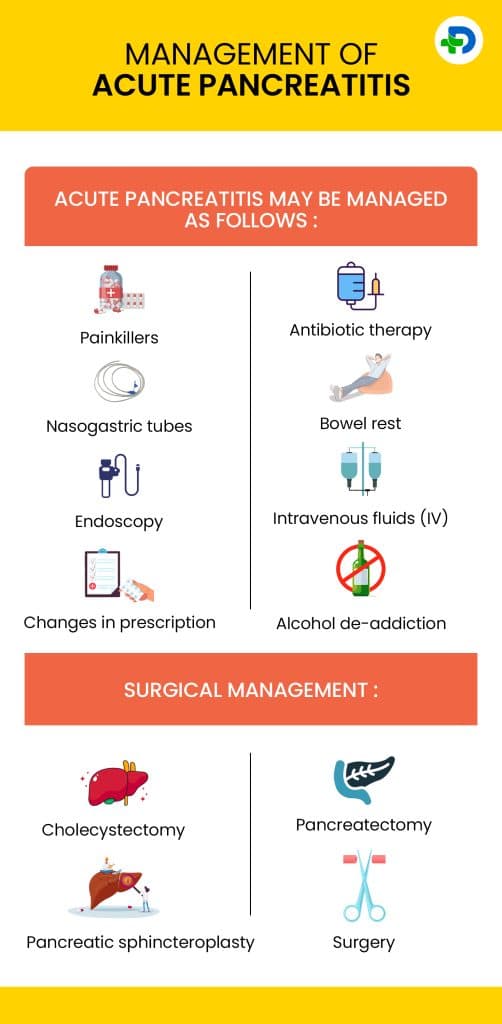
Management of Acute pancreatitis
Acute pancreatitis may be managed as follows:
- Painkillers – Acute pancreatitis may be extremely painful. Pain relievers can be given either as medication orally or through an IV into circulation
- Antibiotic therapy – helps relieve infections
- Nasogastric tubes – can remove extra liquid and air to improve motion sickness and vomiting
- Bowel rest – The gastrointestinal system needs to recover for a few days; thus, the patient won’t be allowed to consume any food or liquids until their condition gets better
- Intravenous fluids (IV): Pancreatitis causes dehydration, and hydration is crucial for healing. In extremely serious circumstances, the doctors may decide to administer nutrition via an intravenous line
- Endoscopy – used to remove gallstones and to sever the sphincter muscle
- Alcohol de-addiction – Enrolling in an alcohol de-addiction program may help reverse the problem in many cases
- Changes in prescription – if a medicine is identified to be the source of acute pancreatitis, the physician may withdraw the medicine and work with the patient to find alternatives
Surgical management:
- Cholecystectomy – done to remove the gallbladder and may help in recurring cases
- Pancreatic sphincteroplasty – done to reconstruct the pancreatic sphincter muscle
- Pancreatectomy – Depending on how severe the problem is, one may need to have the damaged pancreatic tissue removed
- Surgery to eliminate dead tissue or draining fluids
Diet
Dietary modifications
Acute pancreatitis inflammation, complications, and mortality can all be reduced with nutrition supplementation, which also helps avoid malnutrition. 8Dietary modifications | Researched based study from nih.gov
Food recommended for acute pancreatitis :
- Natural low-fat, high-fiber, and antioxidant-rich foods reduce the amount of effort the pancreas must undertake to support digestion.
- Vegetables and fruits
- Whole grains, lentils, and beans
- Fish, including haddock, cod, and other white fish
- Lean meat, such as turkey or chicken
List of foods to avoid:
- Sugary snacks, sweetened beverages, and other refined carbs.
- Alcohol – as it poses a serious risk to those who have pancreatitis.
- High-fat foods, such as fried foods like French fries and potato chips, and high-fat dairy items like cream, whole milk, and full-fat cheeses
- Meats that have been processed, such as hot dogs and sausages.
Takeaway
Key Takeaways
Acute pancreatitis is usually totally reversible and if not serious, the patient should feel better in five to ten days. There is a strong possibility that acute pancreatitis won’t return if a person can prevent what caused it in the future. 20% of those who encounter organ failure die from it. This is a very tiny number of people. It is advisable to visit a doctor for a diagnosis and therapy because one cannot determine the severity of the condition based on its symptoms alone.
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
National Institutes of Health
Pancreatitis/Acute Pancreatitis/Overview
-
National Institutes of Health
Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States/Overview
-
National Institutes of Health
The Epidemiology of Pancreatitis and Pancreatic Cancer/Causes/Gallstones
-
National Institutes of Health
Acute Pancreatitis/Causes/Smoking
-
National Institutes of Health
Global epidemiology and holistic prevention of pancreatitis/Complications/Prevention
-
National Institutes of Health
Dietary Factors Reduce Risk of Acute Pancreatitis in a Large Multiethnic Cohort/Prevention
-
Penn State's College of Information Sciences and Technology
Outcome and Quality of Life in Chronic Pancreatitis/Complications
-
National Institutes of Health
Nutrition management in acute pancreatitis: Clinical practice consideration/Diet





































