Gingivitis Bumps on Gums: Causes, Risk Factors & Management

- Gums
- 15 Sep 2023
Overview
Gum Infection
Periodontal(gum) disease or gingivitis is an inflammation of the gums and bone around the teeth. Poor dental hygiene typically causes it by enabling plaque, a clingy film of microorganisms, to build up on the teeth then harden. Redness, swelling, and bleeding gums are the first signs of gingival infection. If left untreated, chewing can become painful when it extends to the bones close to the gums. In the worst-case circumstances, teeth could deteriorate or need to be removed. 1 Overview | Researched based study from National Institutes of Health

Gingivitis
What is Gingivitis?
- The first stage of gum inflammation (periodontal disease) is gingivitis. It occurs when germs, tartar, and plaque accumulate on your teeth, resulting in red, swollen, and bleeding gums.
- Gingivitis is treatable, especially with a dentist’s assistance. However, it can develop into periodontal disease, an even more serious type of periodontal disease that results in jawbone loss, if left untreated.
- Men are more likely than women to experience related ailments, which may be influenced by hormones.
- People who are uneducated beyond the high school level and those who are in poverty are at high risk.
- Many diseases have links to these factors. Smokers, as tobacco impairs the body’s defenses against infection. Gum disease is quite common. A form of gum disease affects nearly half of all persons over 30. 1Gingivitis | Researched based study from National Institutes of Health
Causes
Causes of Gingivitis
The body’s inflammatory reaction to the deposits of tartar and plaque on the teeth is gingivitis. The gums become inflamed, red, and swollen when calculus and plaque are left on the teeth for an extended period of time. The chance of developing gingivitis may be influenced by the factors listed below:
- Possess hormonal changes that have an impact on oral health, such as pregnancy.
- Have poorly maintained teeth or difficult-to-clean crooked teeth.
- Possess diabetes
- Have a history of gum illness in the family
- Chew or smoke tobacco 2Causes | Researched based study from Cleveland Clinic
Additionally, several over-the-counter and prescription drugs may reduce saliva production, causing dry mouth (xerostomia). Since saliva helps keep the teeth clean, this alteration can make gingivitis worse. Some examples of such drugs are:
- Drug treatments for epilepsy.
- A few cancer treatments.
- Blood pressure medications that inhibit calcium channels.
- Oral birth control. 2Causes | Researched based study from Cleveland Clinic
Communicability
Is Gingivitis contagious?
- It is possible to spread the germs that cause gingivitis from one person to another. Therefore, despite the debate among specialists that gingivitis is not infectious in and of itself, individuals who have the illness can transmit germs through saliva-to-saliva contact.
- Kissing or using the same fork and knife increases the chance of developing gingivitis. However, if you come in contact with saliva from someone who has gingivitis, you are more likely to get it yourself.
- This is especially true if one has poor oral hygiene or health issues like HIV AIDS or leukemia that make one more prone to illness. 2Communicability | Researched based study from Cleveland Clinic
Risk Factors
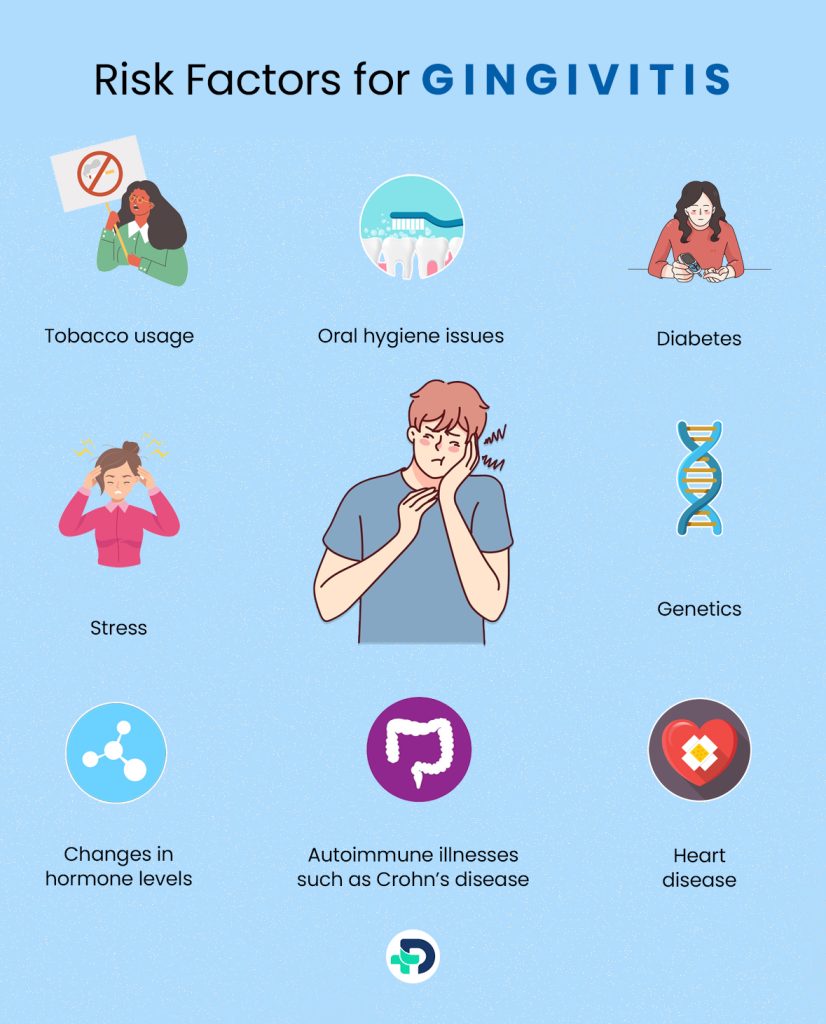
Risk factors for Gingivitis
Anything that raises your probability of contracting a disease or illness is referred to as a risk factor. Risk elements for periodontal disease include:
- Tobacco usage, including smoking
- Oral hygiene issues
- Diabetes
- Stress
- Heart disease
- Genetics 3Risk Factors | Researched based study from National Institutes of Health
- Autoimmune illnesses such as Crohn’s disease, lupus, and scleroderma
- Changes in hormone levels, particularly those that take place during adolescence, menopause, and pregnancy.
Bumps On The Gums
Different bumps present on Gingiva
Among the most frequent lesions observed in patients are gingival lesions, the majority of which are reactive hyperplasia brought on by a variety of persistent irritating stimuli.
Gingival Cyst:
- Adult gingival cysts are a relatively uncommon lesion that makes up a negligible portion (0.2 %) of odontogenic cysts. 4Bumps On The Gums | Researched based study from National Institutes of Health It often manifests in the sixth decade of life and affects more women than males.
- The incisor, canine, and premolar areas of the jaw are the most common locations for these lesions, which often manifest as a painless, blue swelling on the gingiva.
- Canker sores, also known as aphthous ulcers, are shallow and tiny ulcers that develop in the mouth’s lining.
- A canker sore initially appears as a white, yellow, or white-bordered mouth sore. Although they can reach a diameter of one inch or half an inch, they normally possess a diameter of less than one millimeter.
- The tongue, gums, roof of the mouth, within the lip, and under the tongue can all develop canker sores. They often make speech and eating difficult and might hurt.5Bumps On The Gums | Researched based study from Cleveland Clinic
Tori and Exostoses:
- With a frequency of 12 to 15 %, torus palatinus (TP) and the torus mandibularis (TM) are frequent observations in the oral cavity. 4Bumps On The Gums | Researched based study from National Institutes of Health
- They often first appear in young adulthood. In contrast to TM, where men predominate somewhat, TP is twice as prevalent in females.
- Multiple bone nodules called buccal and palatal exostoses are less common than tori. They are more common in men than in women.4Bumps On The Gums | Researched based study from National Institutes of Health
Periodontal Abscess:
- Periodontal abscesses are defined as a localized pus collection within the gingival wall of a gum pocket.
- It occurs more frequently in people who have had prior periodontal pockets and spreads quickly, damaging periodontal tissues and displaying obvious signs.
- The tooth can have a “hopeless prognosis” if it is connected to other abscesses.
- A periodontal abscess is more likely to develop locally when a tooth is invaded, has grooves in the root, is broken, or has external root resorption. 6Bumps On The Gums | Researched based study from National Institutes of Health
Epulis:
- Epulis is an uncommon soft tissue lesion that most frequently appears on the neonates’ anterior alveolar ridge.
- It more frequently affects females and the upper jaw.
- The lesion is often a soft, mucosal-covered lump that ranges in size from a few millimeters to several centimeters and is generally present at birth.
- Large eosinophilic cells having granular cytoplasm forming a submucosal mass are the distinctive histopathological feature. 4Bumps On The Gums | Researched based study from National Institutes of Health
Dentigerous Cyst:
- The most common type of cyst which impacts the jaws is a dentigerous cyst.
- Although these cysts may impact other teeth, they tend to grow around partly erupted wisdom teeth the most commonly. 7Bumps On The Gums | Researched based study from Mayo Clinic
Verruciform Xanthoma:
- The gums and the palate are the most frequent sites for this lesion. 4Bumps On The Gums | Researched based study from National Institutes of Health
Gingival Fibrous Hyperplasia:
- Fibrous hyperplasia, which can account for up to 40 % of mucosal disease in large series, is a fairly prevalent nodule type. 4Bumps On The Gums | Researched based study from National Institutes of Health
- Lesions can develop at any age, although they seem to affect women more frequently.
Peripheral Giant Cell Granuloma:
- With a female predisposition and a lower age incidence rate for males than females, they affect people of all ages.
- Although these lesions can develop anywhere along the gingiva in dentate individuals or on the alveolar ridge in edentulous patients, the majority do so anteriorly to the molar area, with the mandible having a somewhat higher prevalence. 4Bumps On The Gums | Researched based study from National Institutes of Health
Gumboil:
- These lumps, also known as parulis, typically develop around the teeth and move toward the lips and cheeks. They may also be seen on the mouth’s roof.
- When they explode or expel their contents (mainly pus), they are often brought on by a non-vital tooth. Gumboil is an indication that an infected tooth is nearby. 8Bumps On The Gums | Researched based study from MyHEALTH
Ameloblastoma:
- Cells which make up the protecting enamel coating of teeth give rise to this rare, frequently benign tumor. It is usually seen in the jaw, near the molars.
- The most common kind is aggressive and causes large tumors by growing into the jawbone.
- Although recurrence after therapy is possible, extensive surgical treatment will frequently reduce that likelihood. 7Bumps On The Gums | Researched based study from Mayo Clinic
Tips
Tips to reduce the risk of Gingivitis
- By maintaining proper dental hygiene, you can lower your chance of developing gingivitis.
- Once in the morning as well as in the evening, brush the teeth thoroughly.
- To get rid of microorganisms between the teeth, use floss daily.
- Rinsing with mouthwash and similar products can help kill germs that cause illness.
- Take care of your blood sugar level if you have diabetes.
- Avoid smoking or using tobacco products.
- Limit alcoholic and excessive sugary foods and beverages.
- Visit your dentist for checkups at least every year, more regularly if you have any symptoms. The ideal cleaning schedule for you can be determined by consulting your dentist. 2Tips| Researched based study from Cleveland Clinic
- The process known as “scaling and root planing” is comparable to a regular dental cleaning but goes further than the gum line. Tartar and bacteria are removed via scaling. Your teeth’s root surfaces are made smoother by planing, which keeps germs from adhering.
Management
How to treat Gum diseases?
Several variables, such as the following, will determine whether you require surgery or nonsurgical gum disease treatment:
- The gum disease stage
- The present oral condition
- The current general health
- The ability to adhere to oral hygiene recommendations after therapy
There are both nonsurgical and surgical methods for treating gum disease. Additionally, many periodontists use sedation dentistry to make your procedure more pleasant. 9Treatment | Researched based study from Cleveland Clinic
Non-surgical Treatments may include:
Dental Prophylaxis:
- Dental prophylaxis is a regular dental cleaning, similar to the two-yearly appointment that many individuals have with their dentist.
- A dentist cleans the surfaces of your teeth of plaque and tartar during this process.
Scaling & Root Planing:
- Scaling and root planing, a comprehensive dental cleaning, removes plaque as well as tartar from the tooth’s root surfaces down below the gum line.
- Your teeth will be completely cleaned by the dentist or periodontist, who will also smooth down any rough spots on the root of your teeth. This lessens the chance of germs and plaque reattaching.
- In order to make you comfortable and numb your gums throughout this treatment, your periodontist will provide a local anesthetic.
The Use of Antibiotics:
- Antibiotics may be used by your periodontist, either alone or in conjunction with other treatments.
- These drugs can be inserted by your periodontist into the periodontal pocket, which is the region around your teeth and gums.
Periodontal Laser Treatments:
- The periodontist will perform this surgery to remove damaged tissue and eliminate germs under your gums.
- In rare circumstances, medical professionals advise laser treatment instead of conventional gum surgery.
- Laser treatment does not need any incisions or stitches, in contrast to conventional gum surgery. 9Treatment | Researched based study from Cleveland Clinic
Surgical Methods:
Flap Surgery:
- Your periodontist will make incisions along the gum line and then transfer the gums temporarily away from the teeth during this treatment.
- They are able to view the roots underneath because of flap surgery. The tartar accumulation will then be removed, and the root surfaces will be cleaned.
- In other cases, they will reshape and smooth out broken bones to make it more difficult for germs to grow and hide. The gums will then be moved back into place and stitched into position.
A Gum Graft:
- Gum recession, or when the gums slip away from the teeth, is treated with a gum transplant using either one’s tissue, donated tissue, or synthetic tissue.
- A typical sign of periodontal disease is gum recession. The periodontist performs gum grafting surgery, inserting the tissue graft and stitching it into a place where the teeth have receded.
- They will remove the transplant from the roof of the mouth if they are using the patient’s own tissue.
Guided Tissue Regeneration:
- Gaps that develop between the tooth root and bone can be brought on by periodontal disease.
- The periodontist will apply a barrier to the injured area during guided tissue regeneration to prevent gum tissue from developing where the bone should be. This allows the bone surrounding the tooth to regenerate.
- To aid in this process, periodontists frequently implant a bone graft concurrently with the operation. 9Treatment | Researched based study from Cleveland Clinic
Bottomline
Gum Disease-Early care is needed
The chances of maintaining good dental health, in the long run, are higher the earlier you treat gum disease. Gum disease can be treated in its early stages. However, periodontitis’ latter phases harm your gums and the bone beneath them. This causes gaps, or periodontal pockets, surrounding your teeth, which can spread the infection, cause your teeth to become loose, or even cause tooth loss. Numerous factors can cause bumps in the mouth; however, certain bumps may also be symptoms of a sickness. The only way to be certain what these lumps and bumps in the mouth are requires an assessment by an expert in oral and maxillofacial surgery.9Bottomline | Researched based study from Cleveland Clinic
Any feedback on this article?
 This Articles content was accurate
This Articles content was accurate Very Informative Article
Very Informative Article I have a question or a comment
I have a question or a comment
 This article contains inaccurate content
This article contains inaccurate content This article was not helpful
This article was not helpful I have a question or a comment
I have a question or a comment
We appreciate your helpful feedback!
Checkout our social pages
References
-
National Institutes of Health
Overview | Gingivitis
-
Cleveland Clinic
Causes | Communicability | Tips
-
National Institutes of Health
Risk Factors
-
National Institutes of Health
Bumps on the gums
-
Cleveland Clinic
Bumps on the gums
-
National Institutes of Health
Bumps on the gums
-
Mayo Clinic
Bumps on the gums
-
MyHEALTH
Bumps on the gums
-
Cleveland Clinic
Treatment | Bottomline